The Cognitive Effects of Electroconvulsive Therapy in Community Settings
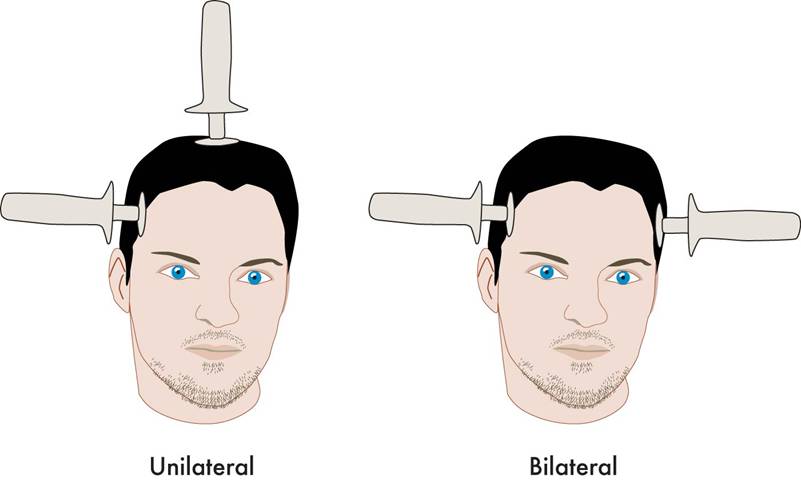
Harold Sackeims’ review in Neuropsychopharmacology, 32, 244-254 (2007) remains one of the best updates indicating that the cognitive effects of Electroconvulsive Therapy (ECT) are not always benign. They followed 347 patients from seven facilities in New York city and tested them after their last session of ECT and then again 6 months later. They reported that “Electrical waveform and electrode placement had marked cognitive effects. Sine wave stimulation resulted in pronounced slowing of reaction time, both immediately and 6 months following ECT. Bilateral (BL) ECT resulted in more severe and persisting retrograde amnesia than right unilateral ECT. Advancing age, lower premorbid intellectual function, and female gender were associated with greater cognitive deficits. Thus, adverse cognitive effects were detected 6 months following the acute treatment course. Cognitive outcomes varied across treatment facilities and differences in ECT technique largely accounted for these differences. Sine wave stimulation and BL electrode placement resulted in more severe and persistent deficits.”
Editors note: This is why it is important to recommend right unilateral ultra brief pulse (RUUBP) ECT both for acute and continuation treatment if necessary. Continuing RUUBP ECT rather than converting to bilateral ECT would appear to be preferable.
AiTBS Superior to ECT in Small Study

Researchers Erica Jensen and Nolan Williams reported in abstracts of a paper that they were to present at the 2020 meeting of the Society of Biological Psychiatry in May that daily sessions of accelerated intermittent theta burst transcranial stimulation (aiTBS) over five or more days produced better results in 15 patients hospitalized for depression and suicidality than in matched patients who received electro-convulsive therapy.
AiTBS is a form of repeated transcranial magnetic stimulation (rTMS), in which a magnetic coil is applied to a patient’s scalp, producing electrical changes in the brain.
The aiTBS treatment was delivered to the left dorsolateral prefrontal cortex. It consisted of 1800 pulses per session, at 80% of a patient’s resting motor threshold with a 50-minute inter-session interval.
The patients in the study were matched (for age, gender, and treatment resistance) to patients who were hospitalized and given ECT. Among patients who received aiTBS and were discharged after an average of 8.4 days, there was an 86% response rate and a 73% remission rate. Among the patients who received ECT, who were discharged after an average of 22.3 days, there was a 53% response rate and a 40% remission rate. With further ECT, response and remission rates increased to 73% and 67%. Time to remission was 3.5 days with aiTBS and 31.3 days for ECT. The investigators concluded conservatively, “Our results suggest that aiTBS could have comparable efficacy to ECT, with potentially faster resolution of acute severe depression.”
Editor’s Note: ECT has been the gold standard treatment for severe depression and suicidality and now we may have a platinum comparator. If these findings are replicated, they could represent a paradigm shift in the treatment of severe depression. Hopefully, this novel form of rTMS will be fast-tracked for approval by the Food and Drug Administration (FDA).
Ultrabrief Right Unilateral ECT Similar in Efficacy to Brief ECT with Fewer Side Effects
 A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
Loo and colleagues analyzed the findings of six different studies that compared right unilateral standard brief pulse ECT with ultrabrief pulse ECT and included a total of 689 patients. Standard ECT was more effective, producing more improvement in mood and more remissions, and working faster than ultrabrief ECT. However, standard ECT also produced greater cognitive side effects in every area tested, including thinking, learning and recall, and memory.
(When bilateral ECT is used, the cognitive effects are even worse, and researcher Harold Sacheim and colleagues have reported that the severity of the impairment in autobiographic memory is directly proportional to the number of bilateral ECT treatments a patient received, even when measured one year after the last session of bilateral ECT. This editor (Robert Post) believes bilateral ECT should be avoided if at all possible, as cognitive side effects can occasionally be severe.)
When Loo and colleagues removed nonrandomized trials from the analysis, the differences in efficacy between ultrabrief and standard right unilateral ECT were not statistically significant. Loo told Medscape Medical News that while the differences in efficacy between brief and ultrabrief ECT are minimal, the differences in side effects are greater. Right unilateral ultrabrief ECT works about as well as standard right unilateral brief pulse ECT, but preserves patients’ cognitive function better.
RTMS in the Elderly and After ECT
At the 2015 meeting of the Society of Biological Psychiatry in May, researcher Daniel Blumberger reported to this editor (Robert M. Post) that he has found repeated transcranial magnetic stimulation (rTMS) to be effective for depression in late life. Blumberger noted that it may be necessary to use higher intensity stimulation (i.e. at 120% of motor threshold instead of the usual 110% of motor threshold) in the elderly in order to overcome the gap between the skull and the brain, which can grow with age due to brain atrophy.
Blumberger has also successfully used rTMS as a followup treatment to a successful course of electroconvulsive therapy (ECT), administering rTMS twice a week for up to 66 treatments in a given patient in order to maintain remission of their depression.
Cognitive Behavioral Therapy an Effective Follow-up to ECT
While electroconvulsive therapy (ECT) is very effective treating acute depression, especially among patients who have not responded to antidepressants, relapse rates following ECT are high. Researchers have been exploring treatments that may extend the effectiveness of ECT and reduce relapses, including antidepressant medication and continuation ECT. A new study by Eva-Lotta Brakemeier and colleagues in the journal Biological Psychiatry finds that cognitive-behavioral therapy combined with medication was most effective at sustaining response to ECT.
In the study, 60 patients who responded well to three-times-per-week right unilateral ultra-brief ECT then were prescribed antidepressant medication following current guidelines for ECT followup. Of these patients, one-third were randomly assigned to receive the medications only. Another third were randomly assigned to receive the medications and continuation ECT, and the final third were randomly assigned to receive medication and participate in 15 weeks of cognitive-behavioral therapy in a group setting. Each group was observed at six months, and then at one year. The group who received medication and cognitive behavioral therapy had significantly higher response rates than the other groups at both follow-up evaluations.
After the initial treatment with ECT, 70% of the patients had responded and 47% had achieved remission. Following the six months of continuation treatment, 77% of the group that received medication and cognitive behavioral therapy responded, while only 40% of the group receiving medication and continuation ECT responded, and 44% of those receiving medication alone responded. After one year (six months following the end of treatment), response rates were 65% for those who had received medication and therapy, 28% for those who had received medication and ECT, and 33% for those who had received medication alone.
Editor’s Note: These results are striking for several reasons. As has been found in most studies, continuation ECT is not very effective at sustaining remission. Cognitive behavioral therapy with medication beats the other options hands-down. These results are in accord with others that show that cognitive behavioral therapy also helps prevent relapses in patients who responded well to medications. The take-home message is that people who respond well to antidepressant medication or ECT would do well to add cognitive behavioral therapy to their other preventive treatments.
The current study did not replicate parameters for continuation ECT that were successful in a study by Axel Nordenskjöld and colleagues in the Journal of ECT in 2013. Nordenskjöld used weekly ECT for six weeks and every two weeks thereafter, for a total of 29 ECT treatments in one year, and found this more intense regimen was more effective at preventing relapse than medication alone.
Investigating Relapse after ECT
 Electroconvulsive therapy (ECT) is an effective treatment for patients with treatment-resistant depression, but still many patients relapse after the treatment. Medications can prolong the period of remission, but even so, relapse rates have increased in recent decades (probably at least partly because ECT was once a standard initial treatment but is now only used with those patients with the most difficult-to-treat illnesses.) A 2013 meta-analysis by Jelovac et al. in Neuropsychopharmacology reviewed existing research on relapse and which medications might be able to best prolong remission after ECT.
Electroconvulsive therapy (ECT) is an effective treatment for patients with treatment-resistant depression, but still many patients relapse after the treatment. Medications can prolong the period of remission, but even so, relapse rates have increased in recent decades (probably at least partly because ECT was once a standard initial treatment but is now only used with those patients with the most difficult-to-treat illnesses.) A 2013 meta-analysis by Jelovac et al. in Neuropsychopharmacology reviewed existing research on relapse and which medications might be able to best prolong remission after ECT.
The researchers analyzed 32 studies that each included at least 2 years of followup. In studies from the recent era in which patients received continuation treatment with medication following ECT, 51.1% of patients relapsed within a year, and the majority of those (37.7%) relapsed within the first 6 months after ECT. Among patients treated with continuation ECT, a similar proportion (37.2%) also relapsed within 6 months of the initial ECT treatment. In randomized controlled trials, treatment with antidepressants with or without lithium following ECT halved the rate of relapse within 6 months compared to placebo.
Even with continuing intermittent ECT treatment, risk of relapse remains high, especially within the first 6 months. The authors concluded that maintenance of wellbeing following ECT must be improved.
Editor’s Note: One possibility for prolonging remission is the more intensive continuation regimen using right unilateral ultrabrief pulse ECT suggested by Nordenskjöld et al. in the Journal of ECT in 2013. Continuation treatment with a combination of ECT and medication resulted in 6-month relapse rates of 29% (compared to 54% with medication alone) and one-year relapse rates of 32% (compared to 61%).
Effectiveness of Continuation Right Unilateral ECT Plus Pharmacotherapy Compared to Pharmacotherapy Alone
A new study is one of the first to find that after successful electroconvulsive therapy (ECT) treatment for depression, continuation of ECT together with pharmacotherapy was superior to continuation with pharmacotherapy alone. ECT produces a seizure while a patient is under anesthesia. The treatment has been successful in acutely treating many patients with severe depression who have not responded to other treatments. The question remains how to maintain the positive acute effects of ECT for a longer duration.
The new research was published in the Journal of ECT in 2013 by Axel Nordenskjöld et al. Patients with unipolar or bipolar depression who improved after an acute series of ECT (usually given 3 times per week) were randomized to receive either continuing ECT plus pharmacotherapy or pharmacotherapy alone. The ECT continuation group received weekly ECT for 6 weeks and every 2 weeks thereafter for a total of 29 ECT treatments in one year. The pharmacotherapy consisted of antidepressants (98%), lithium (56%), and antipsychotics (30%). Venlafaxine (Effexor) was considered the first choice for medication, and lithium augmentation was offered to all patients (not just those with bipolar depression). Of the participants, 64% had recurrent unipolar depression, while less than 20% had bipolar depression.
Among all the patients who were randomized at the beginning of the study (the intent-to-treat cohort), the one-year relapse rate was 61% for patients treated with pharmacotherapy alone and 32% for patients treated with the ECT plus pharmacotherapy (p=0.036). Relapse rates at 6 months were 54% for the pharmacotherapy alone group and 29% for the group receiving ECT plus pharmacotherapy. Some patients required inpatient care during the trial—36% of the patients in the pharmacotherapy alone group and 20% of those in the pharmacotherapy plus ECT group. There was no evidence of a differential effect on cognition across the two groups. (There is concern that bilateral ECT can adversely affect cognition, especially autobiographical memory, but this is not a concern with right unilateral ECT.)
Various parameters for ECT have been studied. This research used unilateral ultrabrief pulse ECT. These parameters are standard in Sweden, where the study took place, and these results are of particular interest as they differ from a US study that used bilateral ECT with treatments given more intermittently. In that study, in which response to ECT with pharmacotherapy did not differ from response to pharmacotherapy alone, ECT continuation was given in the form of 4 weekly treatments, 4 biweekly treatments and then 2 monthly treatments, and this regimen resulted in a relapse rate of 37% within 6 months (Kellner et al. 2006).
Only one other study in geriatric patients who were psychotically depressed showed superiority of continuation ECT.
Editor’s Note: The take-home message from this study may be that for patients with recurrent unipolar depression who respond positively to a course of right unilateral ultrabrief pulse ECT, continuation of regular ECT plus pharmacotherapy is worth considering over pharmacotherapy alone. While direct comparative studies have not been performed, it would appear reasonable to use weekly ECT for 6 weeks and then every 2 weeks thereafter for the continuation ECT treatment rather than a more intermittent series of treatments as in the studies of Kellner et al. Previous studies have shown that the addition of lithium to antidepressants is superior to antidepressants alone in the continuation phase of ECT (Sackeim et al. 2001), so having lithium in the regimen would also appear useful.
ECT Update: Some good news and some not-so-good news
 A 2013 study by Prudic et al. in the Journal of Electro-convulsive Therapy reveals some good and some not-so-good news about ECT. The good news about ECT is that it produced moderate acute remission rates. In this randomized study of ECT treatment, improvement rates were better when patients received right unilateral (RUL) ultra-brief pulse at high doses (6 times a patient’s seizure threshold) than with bilateral (BL) pulse at low doses (1.5 times the patient’s seizure threshold). RUL also has fewer cognitive side effects than BL.
A 2013 study by Prudic et al. in the Journal of Electro-convulsive Therapy reveals some good and some not-so-good news about ECT. The good news about ECT is that it produced moderate acute remission rates. In this randomized study of ECT treatment, improvement rates were better when patients received right unilateral (RUL) ultra-brief pulse at high doses (6 times a patient’s seizure threshold) than with bilateral (BL) pulse at low doses (1.5 times the patient’s seizure threshold). RUL also has fewer cognitive side effects than BL.
Prudic also found that these acute remission rates were best when antidepressant treatment was begun at the same time as ECT rather than after the end of ECT treatment.
Unfortunately, a previous study by Prudic et al. showed that relapse rates after ECT remain high. Two-thirds of patients relapse in the first six months after ECT. Half of patients who receive antidepressant treatment following ECT relapse within the first six months after their last ECT treatment. Twenty to forty percent relapse in the first month after their last ECT treatment.
In the current study, timing and likelihood of relapse was independent of whether antidepressant treatment was started at the outset of ECT or after the end of ECT. Relapse also did not depend on which pharmacological treatments are used (nortriptyine plus lithium versus venlafaxine plus lithium).
Older patients (average age 55) did better—they relapsed less often than patients with an average age of 45. Patients with unipolar and bipolar depression did not differ in relapse rates.
Previous history of illness did affect relapse. The number of prior antidepressant trials a patient had tried for a current depressive episode (a measure of treatment resistance) was related to how fast they relapsed on follow-up pharmacotherapy after receiving ECT (more antidepressant trials was associated with faster relapse).
Other studies have shown that continuation of ECT treatment is not superior to continued treatment with drugs following ECT treatment.
Editor’s Note: ECT works acutely, but too often its effects do not last long, even with intensive continuation treatment with an antidepressant and lithium. Therefore for patients with highly recurrent illness, its usefulness is largely limited to acute emergencies, such as high risk of suicide or medical deterioration.
There are currently no good controlled studies showing how to prevent depressive relapse after remission with ECT using either drug continuation therapy or maintenance ECT. Greater degrees of treatment resistance are associated with lower rates of both acute remission and faster relapse during follow-up pharmacotherapy.
If a patient is going to have ECT, RUL would be recommended over bilateral, because bilateral ECT is associated with decreases in autobiographical memory even after six months, and these deficits are in proportion to the number of bilateral ECT treatments received.
Alternatives to ECT
Other types of brain stimulation treatments could potentially serve as alternatives to ECT. Read more