ECT versus Drug Therapy for Bipolar Depression
 Electroconvulsive therapy is often considered a primary treatment option for patients with severe bipolar disorder that has resisted pharmacological treatment. Researcher Helle K. Schoeyen and colleagues recently published the first randomized controlled trial comparing ECT (in this case right unilateral brief pulse ECT) with algorithm-based pharmacological treatment in 76 patients with treatment-resistant bipolar depression.
Electroconvulsive therapy is often considered a primary treatment option for patients with severe bipolar disorder that has resisted pharmacological treatment. Researcher Helle K. Schoeyen and colleagues recently published the first randomized controlled trial comparing ECT (in this case right unilateral brief pulse ECT) with algorithm-based pharmacological treatment in 76 patients with treatment-resistant bipolar depression.
The response rate was significantly higher in the ECT group than in the patients who received drug treatment (73.9% versus 35.0%). However, the two treatment groups had similarly low remission rates (34.8% for ECT and 30.0% for pharmacological treatment).
The algorithm-based pharmacological treatment used in the study was based on a sequence of treatments endorsed by researchers Frederick K. Goodwin and Kay Redfield Jamison in their 2007 book Manic-Depressive Illness. A selected treatment was chosen for each participant based on his or her medical history. If the first treatment was ineffective or intolerable, the patient would be switched to the next treatment option. Antipsychotics, antidepressants, anxiety-reducing drugs, and hypnotics were some of the other treatments included in the algorithms.
Patients in the study had previously showed a lack of response to at least two different antidepressants and/or mood stabilizers with documented efficacy in bipolar disorder (lithium, lamotrigine, quetiapine, or olanzapine) in adequate doses for a period of 6 weeks (or until they quit because of side effects).
Editor’s Note: Even when ECT is effective, there is the issue of how to maintain that good response. We previously reported that in a 2013 study by Axel Nordenskjöld et al. in the Journal of ECT, intensive followup treatment with right unilateral brief pulse ECT combined with pharmacotherapy was more effective than pharmacology alone at preventing relapses. Patients who improved after an acute series of ECT (three times/week) then received weekly ECT for six weeks and every two weeks thereafter, totaling 29 ECT treatments in one year.
Other studies of more intermittent continuation ECT have not proved more effective than medication. Thus high intensity right unilateral brief pulse ECT is one option for extending the effects of successful ECT.
Investigating Relapse after ECT
 Electroconvulsive therapy (ECT) is an effective treatment for patients with treatment-resistant depression, but still many patients relapse after the treatment. Medications can prolong the period of remission, but even so, relapse rates have increased in recent decades (probably at least partly because ECT was once a standard initial treatment but is now only used with those patients with the most difficult-to-treat illnesses.) A 2013 meta-analysis by Jelovac et al. in Neuropsychopharmacology reviewed existing research on relapse and which medications might be able to best prolong remission after ECT.
Electroconvulsive therapy (ECT) is an effective treatment for patients with treatment-resistant depression, but still many patients relapse after the treatment. Medications can prolong the period of remission, but even so, relapse rates have increased in recent decades (probably at least partly because ECT was once a standard initial treatment but is now only used with those patients with the most difficult-to-treat illnesses.) A 2013 meta-analysis by Jelovac et al. in Neuropsychopharmacology reviewed existing research on relapse and which medications might be able to best prolong remission after ECT.
The researchers analyzed 32 studies that each included at least 2 years of followup. In studies from the recent era in which patients received continuation treatment with medication following ECT, 51.1% of patients relapsed within a year, and the majority of those (37.7%) relapsed within the first 6 months after ECT. Among patients treated with continuation ECT, a similar proportion (37.2%) also relapsed within 6 months of the initial ECT treatment. In randomized controlled trials, treatment with antidepressants with or without lithium following ECT halved the rate of relapse within 6 months compared to placebo.
Even with continuing intermittent ECT treatment, risk of relapse remains high, especially within the first 6 months. The authors concluded that maintenance of wellbeing following ECT must be improved.
Editor’s Note: One possibility for prolonging remission is the more intensive continuation regimen using right unilateral ultrabrief pulse ECT suggested by Nordenskjöld et al. in the Journal of ECT in 2013. Continuation treatment with a combination of ECT and medication resulted in 6-month relapse rates of 29% (compared to 54% with medication alone) and one-year relapse rates of 32% (compared to 61%).
Lithium Discontinuation Results in Only Modest Improvement in Renal Function Compared to Continued Treatment
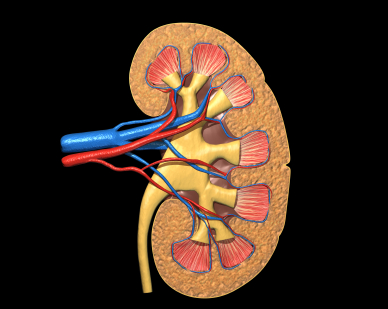 Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Editor’s Note: This study addresses one of the important unanswered questions about what to do when kidney function starts to diminish (observed as high levels of creatinine (Cr) or low Cr clearance) in patients on chronic lithium treatment.
The findings of Rej et al. suggest that the advantages of discontinuing lithium are not huge. Renal function may deteriorate a bit less (or not at all) in those who stop lithium. However, if someone is highly responsive to lithium and the “creatinine creep” upwards is slow, that patient might be able to proceed with careful monitoring and lithium continuation. Where other treatment options are readily available, the discontinuation route might be a good choice.
This study brings some much-needed randomized longitudinal data (if not a definitive recommendation) to bear on a difficult clinical decision that may have to be addressed when lithium is used in long-term approaches to bipolar disorder.

