Red Meat Interacts with Bacteria in the Gut to Raise Heart Disease Risk
 A 2018 study by a group of researchers at the Cleveland Clinic have clarified the way that a diet heavy in red meat may lead to heart disease. The research centers on trimethylamine N-oxide (TMAO), a gut bacteria byproduct that is formed during digestion. When gut bacteria digest choline, lecithin, and carnitine, nutrients that are common in certain animal products and red meat, TMAO is produced.
A 2018 study by a group of researchers at the Cleveland Clinic have clarified the way that a diet heavy in red meat may lead to heart disease. The research centers on trimethylamine N-oxide (TMAO), a gut bacteria byproduct that is formed during digestion. When gut bacteria digest choline, lecithin, and carnitine, nutrients that are common in certain animal products and red meat, TMAO is produced.
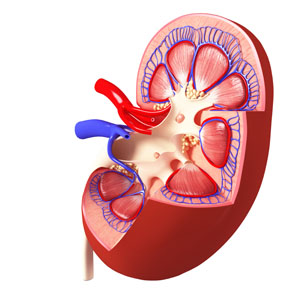
In an article by Robert A. Koeth and colleagues in the European Heart Journal, the researchers show that diets that rely on red meat as the main protein source lead to more circulating TMAO than diets in which white meat or something other than meat is the primary source of protein. They found that in people who eat a lot of red meat, the kidneys are less efficient at expelling TMAO, and levels creep even higher. High levels of TMAO have been linked to hardening and narrowing of the arteries (atherosclerosis) and heart disease complications. High levels of TMAO in the blood can be a predictor of heart attack, stroke, and death.
The study of 113 participants consisted of three different diets that each participant followed in random order (with a washout period in between each diet). A month of eating a diet in which red meat was responsible for at least 25% of participants’ daily calories led to higher levels of TMAO in the blood and urine. TMAO increased threefold during the red meat diet periods compared to periods in which white meat or non-meat protein were the source of those calories, and in certain participants, TMAO increased as much as tenfold. When participants stopped eating the red meat diet, their TMAO levels fell over the following month.
Lithium Has Minimal Effects On Renal Function: Results Of Two New Large Controlled Studies
 Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
Earlier this year we described a 2015 study by Harald Aiff and colleagues that suggested that long-term lithium use was associated with a risk of kidney failure. That study, published in the Journal of Psychopharmacology, included 630 patients who had taken lithium for at least 10 years. One-third of these patients had evidence of kidney dysfunction, and in 5%, the impairment was severe. Two new studies provide some data that suggest these risks may not be lithium-specific and are comparable to risks that come with taking other medications.
The first, by Stefan Clos et al. in The Lancet Psychiatry, included 1,120 patients followed for up to 12 years. On average, these patients had been exposed to lithium for a little over 4.5 years. Clos and colleagues determined patients’ estimated glomerular filtration rate (eGFR), a measure of how well the blood is filtered by the kidneys. The researchers concluded that there was “no effect of stable lithium maintenance therapy on the rate of change of eGFR over time” compared to other drugs such as quetiapine, olanzapine, or valproate.
The second new study, by Lars Vedel Kessing and colleagues in the journal JAMA Psychiatry, included 26,731 patients exposed to lithium and 420,959 exposed to anticonvulsants. Kessing and colleagues concluded that both exposure to lithium and exposure to an anticonvulsant were associated with an increased rate of chronic kidney disease, but lithium was not associated with end-stage kidney disease (the kind that requires dialysis or renal transplantation).
The three studies taken together suggest the following: Taking lithium for an average of 4–5 years does not affect kidney functioning, and longer exposure may not harm kidney function any more than other medications (such as anticonvulsants) would. However, kidney functioning (in terms of eGFR) does decline with age, and is also lower among those with higher baseline eGRF, those with other illnesses, those taking other drugs that affect the kidneys, and those who experience an episode of lithium toxicity. Read more
Long-Term Lithium Treatment Has Risks for Kidney Function, Even with Precautions
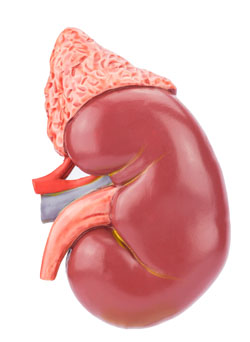 Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
Long-term lithium use has long been associated with decreased renal function. But some Swedish researchers noticed that most long-term studies of patients with renal failure had begun in the 1960s and 1970s. In the 1980s, when it became clear that lithium could reduce renal function, doctors began to institute new safety measures for lithium users, including monitoring of blood levels of the drug and of creatinine, a substance that is excreted by the kidneys as part of normal muscle metabolism. So the researchers undertook a new study to examine whether the protocols instituted in the 1980s had reduced the renal risks of long-term lithium use. Unfortunately, they found that some reduced renal function is still common among people who use lithium for longer than 10 years, and this risk does not necessarily decrease when patients stop taking lithium.
The researchers, led by Harald Aiff, published the study in the Journal of Psychopharmacology in 2015. They identified 4,879 patients who had been prescribed lithium, and narrowed this list down to 630 adult patients who had taken lithium for at least 10 cumulative years, who had normal levels of creatinine when they began taking lithium, and on whom good data existed. About one-third of these patients had evidence of chronic renal impairment, and in 5% of these the impairment was severe or very severe.
Aiff and colleagues’ findings show that lithium treatment requires careful monitoring, especially over the long term. Patients must consider the risk/benefit ratio of lithium treatment. Since prevention of mood episodes can preserve an average ten years of life expectancy, and lithium has the best data for efficacy in preventing manic and depressive episodes, patients must weigh the risks of insufficiently treated bipolar illness against the possibility for long-term decreases in kidney function.
Lithium Discontinuation Results in Only Modest Improvement in Renal Function Compared to Continued Treatment
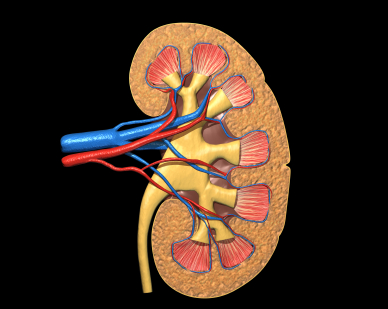 Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Editor’s Note: This study addresses one of the important unanswered questions about what to do when kidney function starts to diminish (observed as high levels of creatinine (Cr) or low Cr clearance) in patients on chronic lithium treatment.
The findings of Rej et al. suggest that the advantages of discontinuing lithium are not huge. Renal function may deteriorate a bit less (or not at all) in those who stop lithium. However, if someone is highly responsive to lithium and the “creatinine creep” upwards is slow, that patient might be able to proceed with careful monitoring and lithium continuation. Where other treatment options are readily available, the discontinuation route might be a good choice.
This study brings some much-needed randomized longitudinal data (if not a definitive recommendation) to bear on a difficult clinical decision that may have to be addressed when lithium is used in long-term approaches to bipolar disorder.
Synthetic Marijuana Comes with Serious Risks, Including Risks to Fetus
Synthetic marijuana, otherwise known as spice, skank, or K2, is not only vastly more potent than the tetrahydrocannabinol (THC) in marijuana plants, but it also lacks cannabidiol (CBD), the calming, antipsychotic substance also present in the plants. This makes spice much more likely to induce major psychiatric effects.
New evidence links use of spice during pregnancy to a tragic birth defect, anencephaly, or absence of the cerebral cortex. It can also lead to the later development of attention-deficit hyperactivity disorder, learning disabilities, memory impairment, depression, and aggression.
of spice during pregnancy to a tragic birth defect, anencephaly, or absence of the cerebral cortex. It can also lead to the later development of attention-deficit hyperactivity disorder, learning disabilities, memory impairment, depression, and aggression.
Effects of THC on gestation may occur as early as two weeks after conception, meaning by the time a woman realizes she is pregnant, the fetus may have been harmed by exposure to the drug.
Other new finding associate use of spice with acute coronary syndrome and the kind of acute kidney injury that can lead to the organ shutting down.
Editor’s Note: It has now been found that synthetic marijuana, or spice, can lead to psychosis, delirium, acute coronary syndrome (heart attack) in young people, and now kidney dysfunction, in addition to causing birth defects if used by pregnant women. Not only is spice made up of more potent THC without the calming effects of CBD, but it is often laced with unknown contaminants, which are likely the cause of the heart and kidney damage.
Smoking regular marijuana is bad enough—it doubles the risk of psychosis and may precipitate the onset of schizophrenia. It may also cause long-lasting effects on cognitive function. Since many states are legalizing marijuana, it is important to know the risks. In any case the risks are much more serious with the synthetic product, and synthetic marijuana should be avoided at all costs.

