Expectations Can Affect Treatment Efficacy
 A 2017 article by Vanda Faria and colleagues in the journal EBioMedicine reports that when patients with social anxiety disorder were told they were being treated with an active drug, they had a response rate three times higher than patients who were given the same drug but told it was an inactive placebo. The researchers suggest that the way treatments are presented to patients affects whether they work.
A 2017 article by Vanda Faria and colleagues in the journal EBioMedicine reports that when patients with social anxiety disorder were told they were being treated with an active drug, they had a response rate three times higher than patients who were given the same drug but told it was an inactive placebo. The researchers suggest that the way treatments are presented to patients affects whether they work.
In the study by Faria and colleagues, patients with social anxiety were given the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram for nine weeks. Some were told they had received escitalopram, while some were told they had received a placebo. Not only did those who were told they were taking escitalopram see greater reductions in their anxiety, they also showed more connectivity between the posterior cingulate and the amygdala, a region that is crucial to mediating anxiety.
This finding is in line with other research that has found that patients’ thoughts and expectations during treatment can affect the efficacy of that treatment.
Researcher Isaac Marks found that patients with obsessive compulsive disorder (OCD) with fear of contamination who were told to avoid things they feared, such as touching a toilet seat, did not fare any better than those taking placebo pills. However, those taking SSRIs who tried new behaviors like touching a toilet seat learned that they could do so without a major fear response, and their phobias improved.
Several studies have shown that expectations of antidepressant efficacy have a big effect on whether patients with unipolar depression improve after beginning treatment with SSRIs. Bret R. Rutherford and colleagues reviewed findings on expectancy in major depressive disorder in a 2010 article in the journal Current Psychiatry Review.
When patients are presented with a drug and encouraged to believe it will work, they may gain the confidence to try out new behaviors or ways of looking at things, whether that means exploring new social situations for someone with social anxiety, or feeling hopeful and breaking the habit of negative rumination for someone with depression. As the study by Faria and colleagues shows, expectations can even change patterns of brain connectivity.
Studies of repetitive transcranial magnetic stimulation (rTMS), in which electromagnets placed near the scalp stimulate electrical impulses in the brain, have shown that patients with depression who engage in positive thoughts and conversations with their rTMS provider during the stimulation improve more than those who sit passively. If a patient engages in their habitual negative ruminations during rTMS, these might even be cemented by the rTMS-induced release of glutamate and brain-derived neurotrophic factor (BDNF), which are both involved in learning and memory processes and what has been called experience-dependent neuroplasticity.
Thus, a patient’s thoughts and outlook during treatment may be important to the therapeutic outcomes achieved. While expectations may not be sufficient to produce an effect on their own, it does seem that thoughts and behaviors can improve a treatment’s efficacy.
A New Treatment for Disruptive Mood Dysregulation
The 2013 update to the Diagnostic and Statistical Manual of Mental Disorders, or the DSM-5, included a new diagnosis of disruptive mood dysregulation disorder. Children with persistent, severe temper outbursts and irritable or angry moods that are out of proportion to circumstances may be diagnosed with the disorder. However, there is not much specificity to the diagnosis and few treatment studies have been done to help clinicians and parents determine how to manage symptoms of the disorder.
A poster presented at the 2017 Psych Congress reported that a medication protocol consisting of an anticonvulsant drug to stabilize moods and temper outbursts and a dopamine agonist to reduce irritability, impulsivity, and concentration problems reduced rates of re-hospitalization. The retrospective study by researchers D. Matthews and G. Matthews included 91 children and adolescents who were prescribed the anticonvulsant oxcarbazepine and the dopamine agonist amantadine following hospitalization for severe aggression, mood instability, and impulsivity. Those who stuck to the regimen with minimal changes for one year had an 8% re-hospitalization rate compared to a 26% re-hospitalization rate among those who discontinued the regimen or substituted other drugs.
Editor’s Note: Oxcarbazepine has a long-acting preparation, Oxtellar, that can be given all at night.
Amantadine (Symmetrel) not only is a dopamine agonist used for Parkinson’s disease, but is also an antiviral and a blocker of glutamate NMDA channels. It stabilizes the closed state of the NMDA channel.
Even Light Exercise Prevents Future Depressions
A 2017 article in The American Journal of Psychiatry suggests that regular leisure-time exercise of any intensity can protect against future depressions.
The study by Samuel B. Harvey and colleagues followed a group of 33,908 healthy adults for 11 years. The researchers found a link between regular leisure-time exercise and reduced incidence of future depression (but not anxiety). This link occurred regardless of the intensity of the exercise, and most of the effect occurred at low levels of exercise. Analysis suggested that 12% of future cases of depression could be prevented if all participants fit one hour of physical activity into their week.
A small part of the benefit came from the social and physical health benefits of exercise.
Harvey and colleagues suggested that from a public health perspective, increasing population levels of exercise modestly could lead to a substantial decrease in depressions.
Editor’s Note: Alongside maintenance treatment, in the form of antidepressants for unipolar depression or mood stabilizers and atypical antipsychotics for bipolar disorder, exercise could provide some benefits in preventing future depressions.
Simvastatin Looks Promising in Treatment of Negative Symptoms of Schizophrenia
The statin drug simvastatin (Zocor) enhances the effects of risperidone on negative symptoms of schizophrenia, according to a 2017 article by Soode Tajik-Esmaeeli and colleagues in the journal International Clinical Psychopharmacology.
In the 8-week study, 40 mg/day of simvastatin enhanced the effects of 4–6 mg/day of the antipsychotic risperidone on negative symptoms of schizophrenia, such as apathy and withdrawal, but not positive symptoms such as hallucinations or delusions.
Other statins, lovastatin and pravastatin, have not had a similar effect, possibly because they do not cross the blood-brain barrier as easily as simvastatin does.
Simvastatin has other benefits as well. Like all statins it decreases lipid levels, reducing cardiovascular disease. People with schizophrenia and bipolar disorder are at especially high risk for cardiovascular disease.
Simvastatin also decreases inflammation (lowering IL-1 alpha and TNF-beta levels) and may be neuroprotective, as it increases brain-derived neurotrophic factor (BDNF), a protein that protects neurons and is important for learning and memory. Inflammation is increasingly implicated in schizophrenia and bipolar disorder.
There is also some evidence that statins can prevent depressions over long-term follow-up. Studies in women without depression and men who had recently had heart attacks both showed that those taking statins had a lower rate of future depression than those not taking statins.
Editor’s Note: These findings suggest a potential 5-fold benefit to simvastatin: 1) It reduces negative symptoms in schizophrenia. 2) It reduces inflammation. 3) It increases BDNF. 4) It decreases cardiovascular disease risk by lowering lipid levels. 5) It may prevent future depressions.
Other approaches to augmenting schizophrenia treatment include nutritional supplements vitamin D3 and folate. Patients with psychosis often have vitamin D deficits. Folate supplements can reduce homocysteine, which has been linked to cognitive deficits in schizophrenia.
Liraglutide Decreased Body Weight, Improved Glucose Tolerance and Cardio Health in Schizophrenia
 A 2017 article by Julie R. Larsen and colleagues in the journal Archives of General Psychiatry reported that the drug liraglutide, a treatment for type 2 diabetes, improved certain health measures in people with schizophrenia who were overweight and prediabetic and being treated with the atypical antipsychotics olanzepine or clozapine.
A 2017 article by Julie R. Larsen and colleagues in the journal Archives of General Psychiatry reported that the drug liraglutide, a treatment for type 2 diabetes, improved certain health measures in people with schizophrenia who were overweight and prediabetic and being treated with the atypical antipsychotics olanzepine or clozapine.
In the 16-week trial, patients received a daily 2 mg injection of liraglutide under the skin or placebo. Liraglutide decreased body weight, improved glucose tolerance, and improved cardio-metabolic measures. Weight decreased by more than 10 pounds on average compared to placebo.
Liraglutide is derived from a human metabolic hormone. It binds to the same receptors as does the metabolic hormone GLP-1, which stimulates insulin secretion.
FDA Approves New Higher Dose of Valbenazine for Tardive Dyskinesia
The US Food and Drug Administration has approved an 80 mg capsule dose of valbenazine (Ingrezza) for tardive dyskinesia (jerky, involuntary movements of the face, especially the mouth and tongue, fingers and body that can be a side effect of antipsychotic medication). Valbenazine, a selective vesicular monoamine transporter 2 inhibitor, was the first drug FDA-approved for tardive dyskinesia. The FDA initially approved a dosage of 40 mg/day in April 2017. The 80 mg/day dose was approved in October 2017.
The new approval was based on a 6-week clinical trial in which 80 mg of valbenazine improved tardive dyskinesia significantly compared to placebo. Improvement continued over 48 weeks of treatment.
Augmentation Strategies for Negative Symptoms of Schizophrenia
In a 2017 article in the journal JAMA Psychiatry, Christoph U. Correll and colleagues reviewed 42 secondary strategies to treat schizophrenia when the primary antipsychotic treatment has an incomplete effect. Many people with schizophrenia show only a limited response to antipsychotic drugs, so additional treatments are often necessary, but currently there are no US Food and Drug Administration guidelines for combination treatment.
Correll and colleagues compiled data from 29 meta-analyses covering 381 individual trials. They found that while the meta-analyses were well done, the quality of the data in the original studies was lacking.
Focusing on Negative Symptoms
However, since the negative symptoms of the illness such as apathy, withdrawal, and blunted emotional response are the hardest to treat, any amount of improvement in this area could be particularly helpful. Read more
Probiotics May Improve Depression As Well As IBS
 A pilot study of people with irritable bowel syndrome (IBS) suggests that taking a probiotic nutritional supplement can improve depression as well as gastrointestinal upset.
A pilot study of people with irritable bowel syndrome (IBS) suggests that taking a probiotic nutritional supplement can improve depression as well as gastrointestinal upset.
In the 2017 study published in the journal Gastroenterology, researcher Maria Pinto Sanchez and colleagues at the Farncombe Family Digestive Health Research Institute found that when those with IBS took a probiotic, their co-occurring depression improved more than it did in people with IBS who took a placebo.
Senior author Premysl Bercik suggested the study confirms that the microbiota environment in the gut affects what goes on in the brain, opening new avenues for the treatment of psychiatric diseases.
The study included 44 adults with IBS who also had mild to moderate anxiety and depression. For 10 weeks, half received a daily dose of the probiotic Bifidobacterium longum NCC3001, while the others received placebo.
After 6 weeks, 64% of the probiotic group saw improvement in their depression, compared to 32% of the placebo group. Functional magnetic resonance imaging (fMRI) showed brain changes associated with the improvement in mood.
The researchers are planning larger trials of probiotics.
TDCS Better Than Placebo But Not as Good as Escitalopram at Improving Unipolar Depression
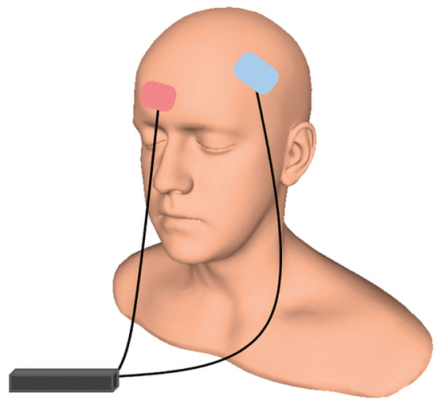 An article by André R. Brunoni and colleagues in the New England Journal of Medicine reports that transcranial direct current stimulation (tDCS) can treat unipolar depression more effectively than placebo, but not quite as effectively as the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram. TDCS consists of a constant, low direct current applied to the scalp via electrodes.
An article by André R. Brunoni and colleagues in the New England Journal of Medicine reports that transcranial direct current stimulation (tDCS) can treat unipolar depression more effectively than placebo, but not quite as effectively as the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram. TDCS consists of a constant, low direct current applied to the scalp via electrodes.
The study included 245 patients with moderate to severe depressive symptoms, many of whom also had anxiety disorders. To minimize the placebo effect, patients all participated in sessions wearing tDCS gear and received a daily pill. However, one group received real tDCS treatment but placebo pills, a second group received sham tDCS but real escitalopram pills, and the third group received both sham tDCS and placebo pills.
The real tDCS treatment consisted of 30-minute sessions of tDCS every day for 15 consecutive weekdays, then seven once-a-week treatments. The escitalopram dosage was 10 mg/day for three weeks, then 20 mg daily.
Ten weeks into treatment, those who received escitalopram showed the greatest improvement in depression. Those who received tDCS showed slightly less improvement, but still significantly more than those who received neither treatment. Cognitive performance either improved or stayed the same in all the groups.
In terms of side effects, those who received escitalopram were more likely to report sleepiness or severe constipation. Those who received tDCS reported more skin redness/tingling, itching, tinnitus, and nervousness. Two patients in the tDCS group had new-onset mania during treatment. There were no suicides, hospitalizations, or other serious side effects.
Taking SSRI Antidepressants May Increase Stroke Risk
 A Taiwanese study published in the Journal of Clinical Psychiatry in 2017 finds that taking selective serotonin reuptake inhibitor (SSRI) antidepressants can increase risk of stroke. The study by Chin-Hong Chan and colleagues analyzed eight years of data from Taiwan’s National Health Insurance Research Database, comparing people who had taken SSRIs for at least two consecutive months to those who had not. First onset strokes were more common among people who had taken SSRIs, and the higher stroke rates in this group persisted for three years after exposure.
A Taiwanese study published in the Journal of Clinical Psychiatry in 2017 finds that taking selective serotonin reuptake inhibitor (SSRI) antidepressants can increase risk of stroke. The study by Chin-Hong Chan and colleagues analyzed eight years of data from Taiwan’s National Health Insurance Research Database, comparing people who had taken SSRIs for at least two consecutive months to those who had not. First onset strokes were more common among people who had taken SSRIs, and the higher stroke rates in this group persisted for three years after exposure.
Ischemic strokes (which occur when a blood vessel carrying blood to the brain is obstructed) were more common than hemorrhagic strokes (which occur when a weak blood vessel ruptures). Younger adult participants exposed to SSRIs were more likely to have strokes, while people older than 65 saw only a slight increase in stroke risk from taking SSRIs. More strokes occurred during the first three years of SSRI treatment than later in treatment.
Chan and colleagues suggest that these strokes are caused by cerebral microbleeding or by overcorrection of hemostasis, the process by which the body slows or stops bleeding by constricting blood vessels and coagulating blood.