Transcranial Direct Current Stimulation (tDCS) Induces Gray-Matter Increases in Depression
At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Mayank Jog and colleagues described a study of transcranial direct current stimulation (tDCS) in 59 patients with moderate depression. The patients received either tDCS sessions that delivered electrical current at 2mA for 20 minutes or a same-length sham stimulation delivered using a double-blind stimulator, for a total of 12 sessions over 12 consecutive working days. Jog and colleagues found that compared to the sham stimulation, tDCS induced increases in gray matter volume in the left dorsolateral prefrontal cortex (DLPFC) target area, with a statistically large effect size (Cohen’s d = 1.3). The researchers plan to follow up this study that found structural changes to the brain after tDCS with more research on the antidepressant effects of the treatment.
Transcranial Direct Current Stimulation Improved OCD in Controlled Trial
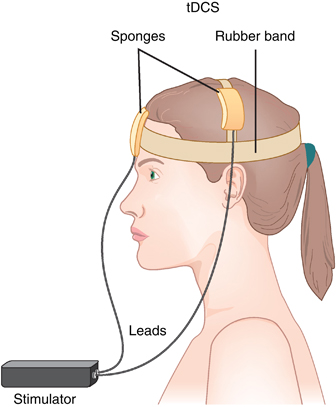
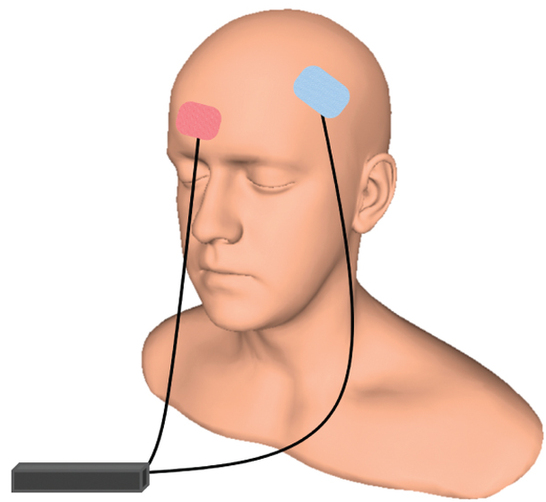
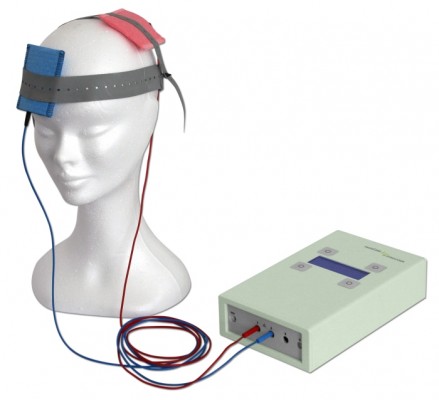
In an abstract of a paper that was to be presented at the 2020 meeting of the Society of Biological Psychiatry in May, researcher Roseli Gedanke Shavitt described a study of transcranial direct current stimulation (tDCS) in people with treatment-resistant obsessive-compulsive disorder (OCD). TDCS is a treatment in which electrodes applied to a patient’s scalp provide a constant low level of electricity that can modulate neuronal activity.
Shavitt and colleagues gave 30 minutes of either active or sham tDCS for 20 days to patients with treatment-resistant OCD. They positioned the cathode over the supplementary motor area of the brain, and the anode over the left deltoid. Those patients who received active tDCS achieved significantly greater reductions in OCD symptoms than did those in the sham group.
30 Minutes of TDCS Better Than 20 Minutes in Patients with Unipolar Depression
 Transcranial direct current stimulation (tDCS) has successfully been used to treat depression. In this treatment, electrodes applied to the scalp provide a constant low level of electricity that can modulate neuron activity. In a 2017 article in the journal Progress in Neuro-Psychopharmacology & Biological Psychiatry, researcher Elena L. Pavlova and colleagues report that both 20- and 30-minute sessions of tDCS improved mild to moderate depression when combined with the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline. However, the 30-minute sessions produced more improvement in depression.
Transcranial direct current stimulation (tDCS) has successfully been used to treat depression. In this treatment, electrodes applied to the scalp provide a constant low level of electricity that can modulate neuron activity. In a 2017 article in the journal Progress in Neuro-Psychopharmacology & Biological Psychiatry, researcher Elena L. Pavlova and colleagues report that both 20- and 30-minute sessions of tDCS improved mild to moderate depression when combined with the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline. However, the 30-minute sessions produced more improvement in depression.
In the study, 69 right-handed patients (average age 37.6) received 50 mg of sertraline (Zoloft) per day and were randomized to one of three tDCS conditions: 10 daily 30-minute sessions, 10 daily 20-minute sessions, or 10 daily sham sessions with no tDCS treatment. The tDCS consisted of 0.5mA anodal current to the left dorsolateral prefrontal cortex.
Both 30-minute and 20-minute tDCS sessions produced greater benefit than the sham sessions. The 30-minute group showed significantly greater percentage improvement in depression scores than the 20-minute group, and included more participants who responded to treatment (89% compared to 68% of the 20-minute group and 50% of the sham group) and more whose depression remitted (70% compared to 27% of the 20-minute group and 35% of the sham group).
TDCS Effective in Bipolar Depression
 A 2017 study in the journal JAMA Psychiatry reports that transcranial direct current stimulation (tDCS) is an effective add-on treatment for bipolar depression. In the study by researcher Bernardo Sampaio-Junior and colleagues, 59 patients taking medication for bipolar disorder and experiencing a depressive episode were randomized to receive either 10 daily half-hour sessions of tDCS (and then one every two weeks) or an inactive sham stimulation.
A 2017 study in the journal JAMA Psychiatry reports that transcranial direct current stimulation (tDCS) is an effective add-on treatment for bipolar depression. In the study by researcher Bernardo Sampaio-Junior and colleagues, 59 patients taking medication for bipolar disorder and experiencing a depressive episode were randomized to receive either 10 daily half-hour sessions of tDCS (and then one every two weeks) or an inactive sham stimulation.
TDCS is a painless form of neurostimulation in which electrodes applied to the scalp provide a steady, low current of electricity that modulates neuron activity. Sampaio-Junior describes its low cost, portability and ease of use as some of its benefits. This is the first randomized, sham-controlled study of tDCS in bipolar disorder.
After six weeks of treatment, patients who received real tDCS treatment showed significantly more improvement in their depression than those who received the inactive sham stimulation. In the active group, 67.6% showed sustained response compared to 30.4% in the inactive group. TDCS was well tolerated, with skin redness at the application site the only side effect that was more common in the active group than in the sham group. Mood switching rates were similar across the two groups.
The research was completed as part of the Bipolar Depression Electrical Treatment Trial (BETTER) taking place in Brazil. The group of participants was 68% female with a mean age of 45.9 years. Sixty-one percent of participants had bipolar I disorder while the remainder had been diagnosed with bipolar II.
TDCS Better Than Placebo But Not as Good as Escitalopram at Improving Unipolar Depression
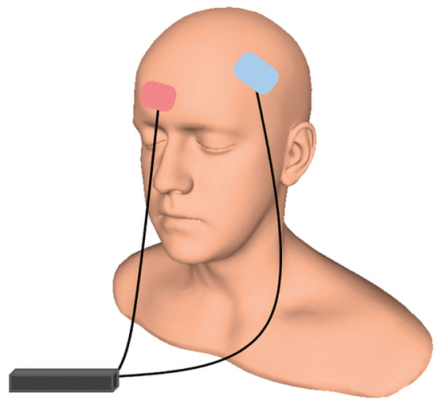 An article by André R. Brunoni and colleagues in the New England Journal of Medicine reports that transcranial direct current stimulation (tDCS) can treat unipolar depression more effectively than placebo, but not quite as effectively as the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram. TDCS consists of a constant, low direct current applied to the scalp via electrodes.
An article by André R. Brunoni and colleagues in the New England Journal of Medicine reports that transcranial direct current stimulation (tDCS) can treat unipolar depression more effectively than placebo, but not quite as effectively as the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram. TDCS consists of a constant, low direct current applied to the scalp via electrodes.
The study included 245 patients with moderate to severe depressive symptoms, many of whom also had anxiety disorders. To minimize the placebo effect, patients all participated in sessions wearing tDCS gear and received a daily pill. However, one group received real tDCS treatment but placebo pills, a second group received sham tDCS but real escitalopram pills, and the third group received both sham tDCS and placebo pills.
The real tDCS treatment consisted of 30-minute sessions of tDCS every day for 15 consecutive weekdays, then seven once-a-week treatments. The escitalopram dosage was 10 mg/day for three weeks, then 20 mg daily.
Ten weeks into treatment, those who received escitalopram showed the greatest improvement in depression. Those who received tDCS showed slightly less improvement, but still significantly more than those who received neither treatment. Cognitive performance either improved or stayed the same in all the groups.
In terms of side effects, those who received escitalopram were more likely to report sleepiness or severe constipation. Those who received tDCS reported more skin redness/tingling, itching, tinnitus, and nervousness. Two patients in the tDCS group had new-onset mania during treatment. There were no suicides, hospitalizations, or other serious side effects.
TDCS May Improve ADHD Symptoms
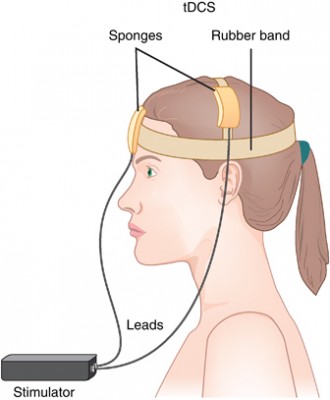 Transcranial direct current stimulation (tDCS) is a therapy in which electrodes placed on the skull deliver a steady, low level current to the brain, changing its threshold for electrical activity. Anodal tDCS to the prefrontal cortex can improve working memory. In a small 2017 study in the Journal of Neural Transmission, Cornelia Soff and colleagues found for the first time that tDCS may improve symptoms of attention-deficit hyperactivity disorder (ADHD).
Transcranial direct current stimulation (tDCS) is a therapy in which electrodes placed on the skull deliver a steady, low level current to the brain, changing its threshold for electrical activity. Anodal tDCS to the prefrontal cortex can improve working memory. In a small 2017 study in the Journal of Neural Transmission, Cornelia Soff and colleagues found for the first time that tDCS may improve symptoms of attention-deficit hyperactivity disorder (ADHD).
People with ADHD tend to have underactivation of the prefrontal cortex and deficits in working memory. The study randomized 15 young people aged 12–16 (three girls and twelve boys) to receive either real tDCS or a sham stimulation. The anodal tDCS was delivered at 1 mA targeting the left dorsolateral prefrontal cortex for 5 days. Those participants who received tDCS showed a reduction in inattention, impulsivity, and hyperactivity compared to those who received the sham stimulation. The effects were more pronounced 7 days after the stimulation, suggesting that tDCS’ effects may be long-term. Larger, more definitive trials are needed to clarify the effects of tDCS on ADHD, but these preliminary findings are promising.
Transcranial Direct Current Stimulation Improved Picture-Naming in People with Dementia
In a study of 12 people with mild Alzheimer’s disease or frontotemporal dementia, transcranial direct current stimulation (tDCS) improved the participants’ abilities to name an object in a picture more than did a sham stimulation. TDCS is a treatment in which an anode and a cathode electrode placed on the skull are used to deliver a steady low level of electrical current to the brain. There is currently no treatment available to specifically target symptoms of dementia such as forgetting words.
The research by Howard Chertkow and colleagues was presented at the 2017 meeting of the American Academy of Neurology. In the study, participants received either 30 minutes of anodal tDCS targeting the parietal lobe of the brain or a sham stimulation.
They also received training in picture-naming. The participants were evaluated before stimulation, at the final stimulation session, two weeks after stimulation, and two months after stimulation. Compared to those who received the sham stimulation, those who received real tDCS improved at picture-naming, and maintained that improvement for two months.
Those who received tDCS also performed better at naming new pictures not included in the training, and were better able to remember a string of digits than those who got the sham stimulation.
TDCS Can Change Sleep Duration
A German study published in 2016 suggests that transcranial direct current stimulation (tDCS) can affect the duration of a person’s nightly sleep. Lukas Frase and colleagues compared the effects of two different tDCS parameters and a sham stimulation on the sleep patterns of 19 healthy volunteers.
TDCS is a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain.
Bi-frontal anodal stimulation, intended to increase arousal, significantly decreased total sleep time compared to the other two interventions.
Bi-frontal cathodal stimulation, intended to decrease arousal, did not increase total sleep time, possibly because there is a ‘ceiling’ beyond which good sleepers do not sleep longer.
EEG analysis showed that the anodal stimulation did increase arousal, while cathodal stimulation decreased it.
The research increases what is currently known about sleep-wake regulation by showing that total sleep time can be decreased using anodal tDCS. The researchers hope this knowledge can contribute to future treatments for disturbed arousal and sleep.
Direct Current Stimulation Improves Negative Symptoms of Schizophrenia
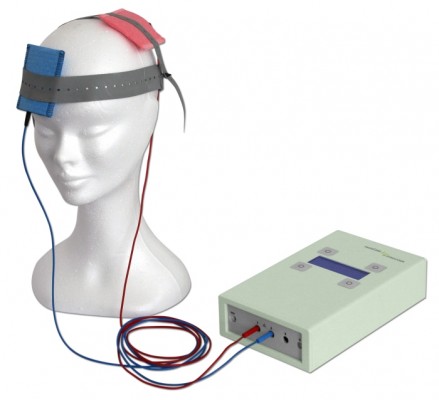 A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
The current study, presented by Ulrich Palm at the 2015 meeting of the Society of Biological Psychiatry, included 20 patients with primarily negative symptoms of schizophrenia, such as thought disorders, poverty of speech, and withdrawal. The patients, who had stable medication regimes for at least three weeks, were randomized to receive either a sham procedure or tDCS with the anode over the left dorsolateral prefrontal cortex and the cathode over the right eye. TDCS stimulation was delivered at a current of 2 mA ten times over two weeks. The patients continued to take their medication and also received functional connectivity magnetic resonance imaging (fcMRI) before and after tDCS treatment.
Two weeks following the stimulation, scores on a scale of positive symptoms (hallucinations and delusions) and negative symptoms of schizophrenia had decreased significantly in those who received tDCS compared to the sham procedure. A measure of negative symptoms was significantly lower among the tDCS group throughout the study period and at the 2-week followup. The fcMRI revealed that those who received tDCS had a deactivated cluster in the brain region that includes the nucleus accumbens, the subgenual cortex, and the striatum.
This study suggests that tDCS is a promising treatment for otherwise difficult-to-treat symptoms of schizophrenia.
Efficacy of Direct Current Stimulation in Major Depression
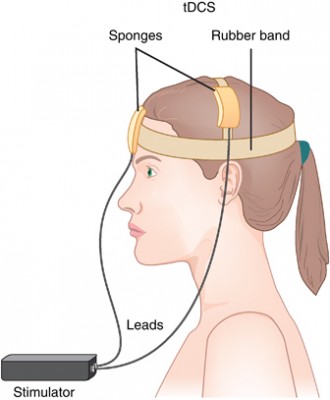 A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
After adjusting for confounding factors, the researchers found that patients who had failed to respond to previous treatments were less likely to respond well to tDCS than other patients. They also found that higher doses of tDCS (in terms of current density, duration, and number of sessions) predicted a better response than lower doses.