Pimavanserin Prevents Relapse in Patients with Dementia-Related Psychosis

At a recent scientific meeting, Erin Foff of Acadia Pharmaceuticals Inc. described a study of pimavanserin (a selective serotonin inverse agonist/antagonist at 5-HT2A receptors) in dementia-related psychosis. Pimavanserin is currently approved in the United States for the treatment of hallucinations and delusions associated with Parkinson’s disease (PD). There is currently no Food and Drug Administration–approved treatment for dementia-related psychosis.
Enrolled patients had moderate-to-severe psychosis associated with Alzheimer’s disease, Parkinson’s, dementia with Lewy bodies, vascular dementia, or frontotemporal dementia. After a 12-week open label phase with flexible dosing and a target dosage of 34mg/day, 217 of the participants with a good response to pimavanserin were then randomized to continue pimavanserin or switch to placebo. The study was stopped early when a prespecified interim analysis revealed that pimavanserin was clearly superior to placebo. There was a more than 2.8-fold reduction in risk of relapse with pimavanserin compared to placebo in the double-blind period. Those on higher doses of 34mg/day showed a more than 3.4-fold reduced risk of relapse. Acadia will seek FDA approval for pimavanserin for the treatment of dementia-related psychosis.
Transcranial Direct Current Stimulation Improved Picture-Naming in People with Dementia
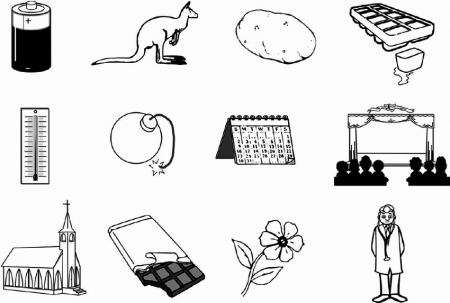
In a study of 12 people with mild Alzheimer’s disease or frontotemporal dementia, transcranial direct current stimulation (tDCS) improved the participants’ abilities to name an object in a picture more than did a sham stimulation. TDCS is a treatment in which an anode and a cathode electrode placed on the skull are used to deliver a steady low level of electrical current to the brain. There is currently no treatment available to specifically target symptoms of dementia such as forgetting words.
The research by Howard Chertkow and colleagues was presented at the 2017 meeting of the American Academy of Neurology. In the study, participants received either 30 minutes of anodal tDCS targeting the parietal lobe of the brain or a sham stimulation.
They also received training in picture-naming. The participants were evaluated before stimulation, at the final stimulation session, two weeks after stimulation, and two months after stimulation. Compared to those who received the sham stimulation, those who received real tDCS improved at picture-naming, and maintained that improvement for two months.
Those who received tDCS also performed better at naming new pictures not included in the training, and were better able to remember a string of digits than those who got the sham stimulation.
Changes in Sense of Humor May Be Warning Sign of Dementia
 A change in a person’s sense of humor could be an early indicator of dementia, according to a 2015 article by Jason Warren and colleagues in the Journal of Alzheimer’s Disease. The changes can appear as early as 10 years before a diagnosis of dementia. Almost all participants who would go on to be diagnosed with frontotemporal dementia showed an increased preference for slapstick humor over satirical or absurdist compared with those who would not. In contrast, changes in sense of humor appeared in less than half of those who would go on to be diagnosed with Alzheimer’s disease, indicating that changes in sense of humor may allow doctors to distinguish between different types of dementia.
A change in a person’s sense of humor could be an early indicator of dementia, according to a 2015 article by Jason Warren and colleagues in the Journal of Alzheimer’s Disease. The changes can appear as early as 10 years before a diagnosis of dementia. Almost all participants who would go on to be diagnosed with frontotemporal dementia showed an increased preference for slapstick humor over satirical or absurdist compared with those who would not. In contrast, changes in sense of humor appeared in less than half of those who would go on to be diagnosed with Alzheimer’s disease, indicating that changes in sense of humor may allow doctors to distinguish between different types of dementia.
The study has some limitations. It was small (48 patients) and relied on patients’ memory of what kind of humor they enjoyed 15 years earlier. More research is needed to clarify the link between changes in humor preferences and dementia.
Warren suggests that changes in humor appear before other warning signs of dementia, such as memory loss. He called humor a type of “stress test” for the brain, since getting a joke can require a quick shift in perspective.