In Animals, Exposure to High Fat Diet During Pregnancy Can Affect Offspring’s Neurological Development
New research in non-human primates suggests that exposure to a high fat diet during pregnancy and in early development prior to weaning can increase the offspring’s propensity for anxiety later in life.
The new research echoes 2010 findings about rats. Researcher Staci D. Bilbo and colleagues reported in the journal of the Federation of American Societies for Experimental Biology that in rats, a high fat diet during pregnancy and lactation led to offspring with greater body weight, increased inflammation, and problems with anxiety and spatial learning. Switching to a standard diet after weaning did not eliminate these outcomes.
The recent research by Jacqueline R. Thompson and colleagues, published in the journal Frontiers in Endocrinology in July 2017, suggests that maternal nutrition in the primate during pregnancy and lactation can have long-lasting effects on offspring’s neurological development, altering the brain and endocrine system. These changes occurred even if the offspring began a normal diet after weaning.
65 female Japanese macaques were divided into two groups, one that received a high-fat diet and one that received a normal diet. In the offspring of mothers who ate a high-fat diet, the researchers found impaired development of neurons containing serotonin. The offspring of the high-fat diet group also showed behavioral alterations such as increased anxiety.
The high rates of obesity in the US and other developed nations make these findings particularly important. The researchers suggest that 64% of women in the US who are of reproductive age are overweight, and 35% are obese. Co-author Elinor Sullivan suggested that the findings from the study could motivate mothers to make healthy nutritional decisions, not only for themselves but for their children as well.
In Mice, Vitamin B3 (Niacin) Prevents Glaucoma
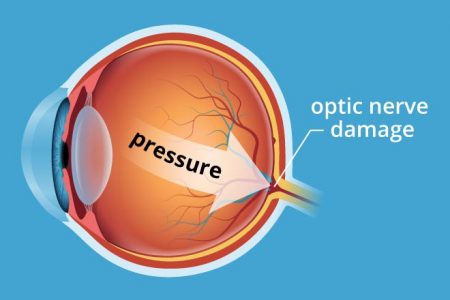
A study published in the journal Science in 2017 reports that adding vitamin B3 to the drinking water of mice prevented them from developing glaucoma. Glaucoma is an age-related condition in which pressure inside the eye damages retinal ganglion cells, the neuronal cells that connect the eye to the brain.
Age contributes both to the buildup of pressure within the eye and to the vulnerability of the neuronal cells to damage. Vitamin B3 seemed to correct the latter problem.
The study by Pete A. Williams and colleagues compared mice with an inherited risk of glaucoma to control mice. Williams and colleagues found that a molecule called NAD that keeps cells functioning normally declined with age, reducing the reliability of the neurons’ energy metabolism.
Vitamin B3 boosted the metabolic reliability of the aging neuronal cells. This helped the cells resist damage from mounting pressure in the eye.
Williams and colleagues also found that a single application of gene therapy with the gene NMNAT1 also prevented glaucoma in the mice. NMNAT1 is the gene for an enzyme that makes NAD from vitamin B3. Gene therapy via an injection in the eye has been approved to treat some rare human eye disorders.
The researchers hope to eventually test vitamin B3 treatment in people with glaucoma and other neurodegenerative disorders.
Editor’s Note: Vitamin B3 may be beneficial for other conditions as well. High-dose niacin (500 mg and up) is a prescription treatment for high cholesterol, and especially the combination of high cholesterol and high triglycerides (blood fats). Niacin may also prevent hardening of the arteries and second heart attacks in men with heart or circulatory problems, and improve diabetes (type 1 and 2). There is some evidence that vitamin B3 can also improve symptoms of osteoarthritis, such as joint stiffness, pain, and swelling. In addition, people who consume more niacin have a lower risk of Alzheimer’s disease, though it is not clear that taking niacin supplements can prevent the illness.
Dutch Study Links Low Vitamin D to Bipolar Disorder
A 2016 study in the Netherlands found that people with bipolar disorder are more likely to have vitamin D deficiency than the general population. Vitamin D deficiency has been linked to other psychiatric disorders including schizophrenia and unipolar depression. Poor diet and lack of exposure to sunlight can put someone at risk for vitamin D deficiency.
The study, led by Remco Boerman and published in the Journal of Clinical Psychopharmacology, included 118 adults with bipolar disorder, 149 with schizophrenia, and 53 with schizoaffective disorder. More than 30% of these participants had deficient levels of vitamin D. Only 15% had optimum levels of the vitamin. More than 22% of the participants with bipolar disorder were deficient in vitamin D, while close to 35% of those with schizophrenia and schizoaffective disorder were deficient.
Study participants had vitamin D levels that were 25% lower than those of the white Dutch population, and vitamin D deficiency was 4.7 times more common in those with psychiatric disorders than the general Dutch population.
The authors suggested screening people with bipolar disorder, schizophrenia, and schizoaffective disorder for low levels of vitamin D.
Giving Infants Vitamin D Can Reduce Type 1 Diabetes
 A 2001 cohort study in Finland showed that giving vitamin D supplements to infants may reduce their risk for type 1 diabetes. The data for the study, by Elina Hyppönen and colleagues in the journal The Lancet, came from 10,366 people born in 1966. Their mothers were part of a medical registry that collected information on vitamin D given to children during the first year of their lives.
A 2001 cohort study in Finland showed that giving vitamin D supplements to infants may reduce their risk for type 1 diabetes. The data for the study, by Elina Hyppönen and colleagues in the journal The Lancet, came from 10,366 people born in 1966. Their mothers were part of a medical registry that collected information on vitamin D given to children during the first year of their lives.
Of the 10,366 people in Hyppönen’s study, 81 had been diagnosed with type 1 diabetes by the end of 1997. Those participants who were given vitamin D supplements during their first year of life were less likely to be diagnosed with type 1 diabetes than other participants. Those who regularly took the recommended dose at the time, 2000 IU daily, during their first year of life had significantly lower diabetes rates 33 years later.
Vitamin D Supplementation May Not Be Effective in Bipolar Depression, But Is Still Worth Doing
 In some studies, vitamin D supplementation (1,500 IU/day) has been found to improve unipolar depression. Recently, researchers led by Wendy K. Marsh found that compared to placebo, 12 weeks of vitamin D3 supplementation (5,000 IU/day) did not produce greater improvement in depressive symptoms. The study, presented at the 2016 meeting of the Society of Biological Psychiatry, included 33 adult participants whose vitamin D levels remained deficient throughout the study.
In some studies, vitamin D supplementation (1,500 IU/day) has been found to improve unipolar depression. Recently, researchers led by Wendy K. Marsh found that compared to placebo, 12 weeks of vitamin D3 supplementation (5,000 IU/day) did not produce greater improvement in depressive symptoms. The study, presented at the 2016 meeting of the Society of Biological Psychiatry, included 33 adult participants whose vitamin D levels remained deficient throughout the study.
Editor’s Note: Caution is urged in interpreting this small study, especially because the participants did not achieve healthy levels of vitamin D.
Low levels of vitamin D are common in children and adults with bipolar disorder. Future research may explore whether raising vitamin D levels to healthy levels has a beneficial effect on mood. There are many other benefits to vitamin D supplementation. It can improve cognition, regulate calcium and phosphorus absorption, and maintain healthy bones and teeth. It may also protect against diseases such as cancer, type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and Crohn’s disease. Improved cardiovascular health is also a possible benefit of vitamin D supplementation.
Omega-3 Fatty Acids May Be Helpful Early in Schizophrenia, But Not Later
 Some studies have suggested that omega-3 fatty acids may be helpful in the treatment of schizophrenia, but data to support this idea have been inconsistent. A recent meta-analysis of research on omega-3s and schizophrenia suggests that this nutritional supplement might be more useful in early-stage schizophrenia than in later illness.
Some studies have suggested that omega-3 fatty acids may be helpful in the treatment of schizophrenia, but data to support this idea have been inconsistent. A recent meta-analysis of research on omega-3s and schizophrenia suggests that this nutritional supplement might be more useful in early-stage schizophrenia than in later illness.
At the 2016 meeting of the Society of Biological Psychiatry, researchers led by Alexander T. Chen presented the findings of their meta-analysis. First they analyzed six studies that shared a common scale for measuring schizophrenia symptoms. In these studies, omega-3 fatty acids did not outperform placebo when used as an add-on treatment to antipsychotics for people with schizophrenia.
In four remaining studies of omega-3 fatty acids and schizophrenia, the omega-3s were associated with improvement only in patients in the early stages of schizophrenia. Compared to placebo, the supplements decreased non-psychotic symptoms, decreased the dosage of antipsychotic medication patients required, and improved early treatment response (but not late treatment response) in patients in their first episode of schizophrenia.
In the same study, omega-3 fatty acids also reduced conversion to full-blown schizophrenia and psychotic symptom severity in patients at high risk for schizophrenia who were having preliminary symptoms of the illness.
Editor’s Note: Researcher Paul E. Keck has also found that omega-3 fatty acids may be more effective early in bipolar disorder rather than later. He reported that younger patients with bipolar depression and rapid cycling showed more improvement when taking the omega-3 fatty acid EPA than when taking placebo. In contrast, patients with bipolar depression who were over the age of 45 did worse on EPA than on placebo.
Part of the ambiguity about whether omega-3 fatty acids can help treat or prevent mental illness may be explained by the supplements working better in younger people or earlier in the course of an illness.
Folate Fortification in Commercial Foods Led to Greater Cortical Thickness
 In 1996, the US began to require that enriched cereal grain products be fortified with folate, a vitamin that is particularly important to fetal brain development. A new study of children born before and after this policy change suggests that the increased folate in commercial foods after 1996 led to increases in cortical thickness in the children born after the change.
In 1996, the US began to require that enriched cereal grain products be fortified with folate, a vitamin that is particularly important to fetal brain development. A new study of children born before and after this policy change suggests that the increased folate in commercial foods after 1996 led to increases in cortical thickness in the children born after the change.
At the 2016 meeting of the Society of Biological Psychiatry, Joshua L. Roffman and colleagues described their research into the effects of folate fortification. The researchers identified 3,309 children born between 1993 and 2001 who had had a magnetic resonance imaging (MRI) brain scan. Analysis of the scans showed that children born after folate fortification began had thicker cortices than those born before the change. The frontal and temporal regions of the brain were particularly affected.
A thin cortex is a risk factor for schizophrenia and other cognitive problems.
Editor’s Note: Folate supplementation has also been shown to enhance the effects of selective serotonin reuptake inhibitor (SSRI) antidepressants in adults with lingering symptoms of depression.
Up to a third of the population may have a deficit of MTHFR, an enzyme important for folate metabolism, and for these people, l-methylfolate is recommended rather than folate itself.
Vegan Diet Can Lead to Vitamin B12 Deficiency
Vitamin B12 deficiency is a risk associated with a vegan diet. B12 deficiency can lead to depression, anemia, and even irreversible neuron damage, according to researcher Drew Ramsey, who spoke on the topic at the 2016 meeting of the American Psychiatric Association.
A study of vegans showed that 52% were deficient in vitamin B12, while another 23% had insufficient levels of the vitamin. B12 is found in the highest concentrations in certain seafoods and liver. It is also found in dairy products, eggs, fortified breakfast cereals, and is available in supplement form.
Women who eat a vegan diet while pregnant may not be providing their offspring with enough nutrients, according to researcher Emily Deans, who also spoke at the meeting. A case report on 30 vegan mothers found that 60% of their offspring had developmental delays and 37% showed cerebral atrophy.
Deans said that eating no meat is associated with higher rates of depression, anxiety, and worse quality of life.
Ramsey believes that while the North American diet is probably weighted too heavily toward animal products, seafood remains an important source of B12.
Eat More Plants for Health
A long-term study of 130,000 nurses and other health professionals found that eating more plants lowered risk of death over several decades. A 3% increase in calories from plant protein was associated with a 10% lower risk of death during the study period.
The research, by Mingyang Song and colleagues in the journal JAMA Internal Medicine, found that the more animal protein consumed, the higher the risk of death from cardiovascular disease during the study. A 10% increase in the proportion of calories from animal protein was associated with a 2% increase in deaths. This association was worse for people who were obese or heavy drinkers.
Song and colleagues suggest that plants are a better source of calories than are animal products, and that fish or chicken are better choices than processed red meat.
Researcher Dariush Mozaffarian recommends eating plant-based foods like fruits, nuts, seeds, beans, and non-starchy vegetables, but avoiding those like French fries or white bread that have little nutritional value.
Metabolized Form of B Vitamin Improves Depression in People with MTHFR Deficiency
MTHFR is an enzyme needed for the body to break down vitamin B9, also known as folate or folic acid. It also helps convert the toxic amino acid homocysteine into the antidepressant amino acid s-adenysl-methionine. However, a significant segment of the population (some estimate 40%) have a genetic mutation in the MTHFR gene that interferes with the body’s ability to break down B vitamins and is linked to higher levels of homocysteine. MTHFR mutations are also linked to depression.
A 2016 study by Arnold W. Mech and Andrew Farah in the Journal of Clinical Psychiatry found that treating people with major depression and a MTHFR deficiency using a combination of micronutrients and already-broken-down B vitamins improved their depression and reduced their homocysteine levels compared to placebo.
The study included 330 adult patients with major depression and one of two genetic variants in the MTHFR gene—C677T or A1298C. Of those who received the metabolized vitamins, 82.4% showed reduced homocysteine levels. Those who received placebo showed a small average increase in homocysteine. The vitamin group also saw a large drop in depression symptoms on average after 8 weeks, with 42% achieving full remission. There were no side effects.
These findings suggest that homocysteine levels play a role in depression and that metabolized B vitamins can be an effective treatment for depression, particularly in those with a MTHFR deficiency. A metabolized form of folate that is commercially available is called L-methylfolate.