Bipolar I patient show dramatic reductions in white matter integrity
Thiel et al in Neuropsychopharmacology (2024) reported that “Compared with HC [healthy controls], BD-I patients exhibited lower FA [fractional anisotropy] in widespread clusters (ptfce-FWE?< 0.001), including almost all major projection, association, and commissural fiber tracts. BD-II patients also demonstrated lower FA compared with HC, although less pronounced (ptfce-FWE?=?0.049).”
Editors Note: These data once more emphasize the importance of using lithium (Li) in bipolar disorder as it can ameliorate the deficits in white matter integrity that are so prominent in the illness. Li also improve the loss of cortical grey matter volume that evolves with illness progression. Li prevents episodes of depression and mania and reduces the incidence of suicides. That Li can reverse or ameliorate brain abnormalities in bipolar disorder is one more piece of evidence that Li should be considered a disease modifying drug (DMD) and started early in the course of illness in almost all bipolar patients. The new mantra for patients and clinicians is: Use more lithium and prevent illness progression.
Changes in brain structure in remitted bipolar patients
Macoveanu et al reported in the Journal of Affective Disorders (2023) that compared to controls that remitted bipolar patients had “a decline in total white matter volume over time and they had a larger amygdala volume, both at baseline and at follow-up time. Patients further showed lower cognitive performance at both times of investigation with no significant change over time….Cognitive impairment and amygdala enlargement may represent stable markers of BD early in the course of illness, whereas subtle white matter decline may result from illness progression.”
Long COVID ‘Brain Fog’ Confounds Doctors, but New Research Offers Hope
James C. Jackson, PsyD, a licensed psychologist specializing in neuropsychology and rehabilitation, at Vanderbilt University School of Medicine and author of a new book, Clearing the Fog: From Surviving to Thriving With Long COVID ? A Practical Guide, reports in Medscape July, 2023 : “There’s not a lot of imprecision in the term (brain fog) because it might mean different things to different patients,”
Jackson, who began treating [a patient] in February 2023, said that it makes more sense to call brain fog a brain impairment or an acquired brain injury (ABI) because it doesn’t occur gradually. COVID damages the brain and causes injury. For those with long COVID who were previously in the intensive care unit and may have undergone ventilation, hypoxic brain injury may result from the lack of oxygen to the brain.
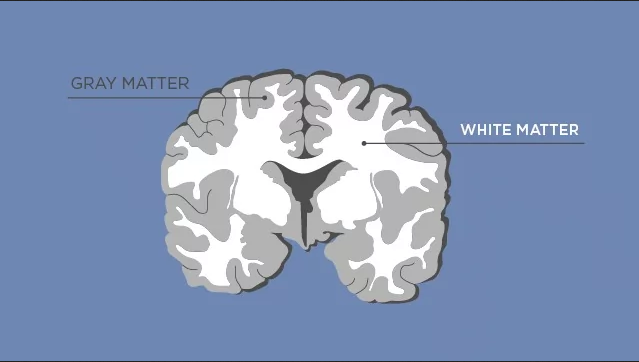
An April 2022 study published in the journal Nature found strong evidence that SARS-CoV-2 infection may cause brain-related abnormalities, for example, a reduction in gray matter in certain parts of the brain, including the prefrontal cortex, hypothalamus, and amygdala.
Additionally, white matter, which is found deeper in the brain and is responsible for the exchange of information between different parts of the brain, may also be at risk of damage as a result of the virus, according to a November 2022 study published in the journal SN Comprehensive Clinical Medicine.“
Thus, new data suggest that long COVID is associated with inflammation and both reduced volume of several brain structures and decreases in white matter. These data suggest several novel approaches to therapy that require further study. One is low dose lithium which both increases gray matter volume and white matter integrity. Lithium also has some antiviral properties. This could be combined with anti-inflammatories that could be bought over the counter such as N-acetylcysteine (NAC), acetyl-L-carnitine, and celecoxib.
Note of caution. This is only an untested hypothesis and would need to be discussed with one’s physician before any of these options are considered.
Both Obesity and Bipolar Disorders in 2249 Individuals Show White Matter Microstructure Abnormalities
Lorielle Dietze of Dalhousie University “obtained body mass index (BMI) and diffusion tensor imaging derived fractional anisotropy (FA) values from 930 individuals with bipolar disorders (BD), and 1319 control individuals from 20 cohorts in the ENIGMA-BD Working Group.”
They “found that lower FA was associated with both BD and BMI, in five white matter tracts, including the corpus callosum and thalamic radiation. Nine ROIs were correlated with only BD, while higher BMI was uniquely correlated with lower FA in four white matter ROIs.”
They concluded: “For the first time we showed that both obesity and BD demonstrated lower FA in some of the same regions. The impact of obesity may be greater in some tracts in BD individuals.”
Cognitive Function and White Matter Integrity in Individuals With Bipolar Disorder
Highlights from Posters Presented at the Society of Biological Psychiatry Meeting, April 27-29, 2023 in San Diego
Jennifer McDowell reported that they found “significantly reduced FA (fractional anisotropy) values in 85 bipolar probands compared to 66 controls” in multiple (n=8) white matter tracts. There were significantly lower scores in bipolar probands compared to controls on composite scores, ( p = 0.007), verbal fluency, ( p < 0.001), and symbol coding, (p = 0.023). They concluded that: “ Impacted connectivity in critical fiber tracts may be key to understanding the neural underpinnings of deficits, like cognition, observed in this clinical population.”
Editors note: It is of interest that lithium has been shown to normalize some white matter abnormalities in youngsters and help preserve cognitive function in older individuals. On this and many other accounts, way too little lithium is being used in the treatment of patients with bipolar disorder. Lithium not only increases neurogenesis (new grey matter neurons) and hippocampal volume, but also has positive effects on white matter tracts and even increases the length of one’s telomeres (which keeps you more healthy). In other ungrammatical words, “If your brain is not connected right, it don’t work right.”
White Matter Disturbances in Bipolar Disorder
At the 2020 meeting of the International Society for Bipolar Disorders, researcher Clare Beasley described the cellular and molecular underpinnings of the white matter abnormalities typically seen in children and adults with bipolar disorder. Researchers consistently see white matter abnormalities in neuroimaging studies of bipolar disorder, but not much is understood about what creates these deficits.
Beasley and colleagues studied autopsy specimens and found that compared to controls, people with bipolar disorder had a number of abnormalities affecting glial cells, lipid composition, and axons.
The researchers found increased density of oligodendrocytes (glial cells that produce the myelin that wraps around axons, the long fibers of nerve cells where impulses travel out to other cells) and an associated protein called CNP in the prefrontal cortex. The myelin is what makes up white matter, while gray matter consists of cell bodies of neurons and glial cells.
People with bipolar disorder also had differently-shaped astrocytes, another type of glial cell that abuts synapses. The researchers found changes in lipid composition, including phospholipid and fatty acid levels, in the white matter of people with bipolar disorder. There were also problems with axons. Beasley and colleagues noted lower density of axon-associated proteins, which are involved in transport of substances along the axons in people with bipolar disorder.
The authors conclude that these data implicate specific disturbances in oligodendrocytes and axonal function associated with the white matter alterations usually seen in neuroimages of people with bipolar disorder.
Inflammation Predicts Lower Frontal and Temporal White Matter Volumes in Early-Stage Bipolar Disorder
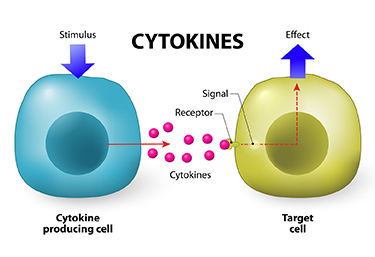 At the 2019 meeting of the International Society for Bipolar Disorders, researcher David Bond found that seven inflammatory cytokines predicted lower white matter volumes in the left frontal and bilateral temporal lobes, as well as in the cingulate and inferior frontal gyri. Cytokines are secreted by some immune cells and send signals that can produce an effect in other cells.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David Bond found that seven inflammatory cytokines predicted lower white matter volumes in the left frontal and bilateral temporal lobes, as well as in the cingulate and inferior frontal gyri. Cytokines are secreted by some immune cells and send signals that can produce an effect in other cells.
Bond noted that greater inflammation did not predict lower parietal or occipital white matter volumes, suggesting that inflammation had a greater effect on white matter volume in those parts of the brain most closely linked to mood disorders.
Lithium Reverses Some White Matter Abnormalities in Youth with Bipolar Disorder
 Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Editor’s Note: This is another reason to consider the use of lithium in children with bipolar disorder. Lithium treatment may help normalize some of the earliest signs of neuropathology in the illness.
White Matter Abnormalities in Obesity
Researcher Ramiro Reckziegel and colleagues reported at a recent scientific meeting that white matter is abnormal in obese adults with bipolar disorder. In a 2018 article in the journal Schizophrenia Bulletin, Reckziegel reported that body mass index (BMI) was associated with reduced fractional anisotropy, a measure of brain fiber integrity, in the cingulate gyrus in patients with bipolar disorder. This finding implies that obesity may play a role in white matter microstructure damage in the limbic system.
White Matter Abnormalities Linked to Irritability in Both Bipolar Disorder and DMDD
 At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.


