Environmental Influences on Gene Structure May Be Transmitted to Offspring
It has been thought that one fundamental principle of genetics is that the impact of environment factors cannot be passed from one generation to the next via the genetic code. New data suggest this may not be true.
In an emerging field called epigenetics, researchers are finding that while the impact of environment and life experiences is not registered in DNA sequences, environmental factors can influence the structure of DNA or tightness of its packaging. Early life experiences, particularly psychosocial stress, can lead to the accumulation of methyl groups on DNA (a process called methylation), which generally constricts DNA’s ability to start transcription (turning on) of genes and the synthesis of the proteins the genes encode. DNA is tightly wound around proteins called histones, which can also be methylated or acetylated based on events in the environment. When histones are acetylated, meaning that acetyl groups are attached to them, DNA is wound around them more loosely, facilitating gene transcription (i.e. the reading out of the DNA code into messenger RNA, which then arranges amino acids in order to construct proteins). Conversely, histone methylation usually tightens the winding of DNA and represses transcription.
Inflammation in the Affective Disorders
Bipolar children exhibit more inflammation than healthy children, according to a paper presented by Pandey, Dwivedi, and Pavuluri from the University of Illinois at the American College of Neuropsychopharmacology in December 2009.
In “Pro-inflammatory cytokines in plasma of patients with pediatric bipolar disorder,” the researchers described their study in which 21 normal controls were compared with 22 children with pediatric bipolar disorder who were unmedicated for a period of at least two weeks. The level of the inflammatory cytokine interleukin-1b (IL-1b) was significantly higher in the pediatric bipolar patients compared with controls, and levels of TNF alpha, another inflammatory marker, were significantly higher as well. Not only is this evidence of increased inflammatory processes in pediatric bipolar disorder, but TNF alpha is associated with activation of transcription factors and the initiation of preprogrammed cell death, or apoptosis.
Episodic vs. Continuous Social Stress Result in Different Rates of Cocaine Use
In a study of rodents exposed to stress (by being forced to enter another rodent’s territory) and given the opportunity to self-administer cocaine, those exposed to a few brief episodes of stress increased their cocaine use and engaged in binge-like episodes, while those exposed to stress chronically showed suppressed cocaine use.
At the American College of Neuropsychopharmacology meeting in December 2009, Klaus Miczek and colleagues from Tufts University in Boston presented a fascinating study indicating that the temporal aspects of the experience of social stress may have dramatic impact not only on defeat stress behaviors and the associated biochemistry, but also on the likelihood that an animal adopts cocaine self-administration. These investigators compared episodic versus chronic defeat stress in rodents.
Episodic social defeat stress consisted of four brief confrontations between an intruding animal and an aggressive resident rat over the course of a period of ten days. In contrast, chronic subordination stress involved the continuous exposure of the intruder rat to an aggressive resident over five weeks, during which time the intruder lived in a protective cage within the resident’s home cage.
The episodically defeated intruder rats showed increases in intravenous cocaine self-administration and prolonged binge-like episodes, along with increases in brain-derived neurotropic factor (BDNF), which is necessary for long-term learning and memory, in the midbrain ventral-tegmental area (VTA) and increased dopamine release in the nucleus accumbens, the reward area of the brain. In contrast, the continuously subordinate rats showed the opposite pattern of suppressed cocaine intake, suppression of dopamine release in the n. accumbens, and reduced BDNF in the VTA.
Persistence of Mild Depression Is Risk Factor for Relapse into Full-Blown Episodes
In naturalistically treated bipolar patients, depression is three times more prevalent than manic symptoms (according to studies by Judd et al., Kupka et al., and Ezquiaga et al.). The occurrence of even residual depression or subsyndromal symptoms can be highly impairing, and is a predictor of increased likelihood for subsequent relapse, according to a poster presented by Gitlin et al. at the American Psychiatric Association meeting in San Francisco in May 2009.
These new data support that of a large number of other investigators who have made similar observations, all indicating the importance of attempting to achieve full remission as a major goal of clinical therapeutics in order to decrease likelihood of relapse. Gitlin’s study further indicated that impairment of quality of life in bipolar patients was closely related to the degree of their subsyndromal symptomatology.
Latest BNN is available in our Archives!
We’ll be posting all of the articles from the latest print BNN over the next week or so, but in the meantime if you’re looking for an article from the latest BNN, check our Archives! You can download a PDF of the print version.
Brain Stimulation for Treatment-Resistant Depression
There are many methods of stimulating the brain directly, ranging from the very invasive to the non-invasive. Below we discuss deep brain stimulation, frontal lobe and vagal nerve stimulation, repeated transcranial magnetic stimulation, electroconvulstive therapy (in particular the new right unilateral ultra-brief pulse method), and low level magnetic fields.
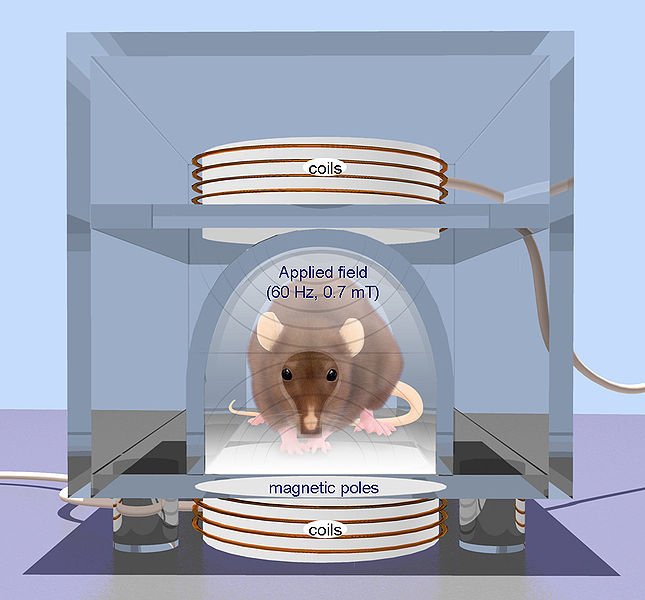
- Repetitive transcranial magnetic stimulation (rTMS) is a technique for noninvasive stimulation of the adult brain. Stimulation is produced by generating a brief, high-intensity magnetic field by passing a brief electric current through a magnetic coil. Compared with the growing number of clinical trial with rTMS, there are surprisingly few animal studies on its basic mechanisms of action, constraining the ability to perform hypothesis-driven clinical studies.
This is an Open Access image distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. From: Arias-Carrión International Archives of Medicine 2008 1:2 doi:10.1186/1755-7682-1-2
Deep Brain Stimulation
At the American Psyciatric Association meeting in San Francisco in May 2009, Giacobbe et al. reported on the results of deep brain stimulation of an anterior-ventral part of the prefrontal cortex called the subgenual cingulate cortex in patients with refractory major depressive disorder. In deep brain stimulation, electrodes are inserted directly into the brain. Twenty-one patients received this treatment in an open study at sites in Canada at McGill University, the University of British Columbia, and the University of Toronto. This multi-center trial replicated results reported by Mayberg et al. (2005) with stimulation of what is also called Broadman’s area 25, or the part of the prefrontal cortex just under the anterior part of the corpus callosum (which carries fiber tracts between the left and right sides of the brain).
Read more
Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
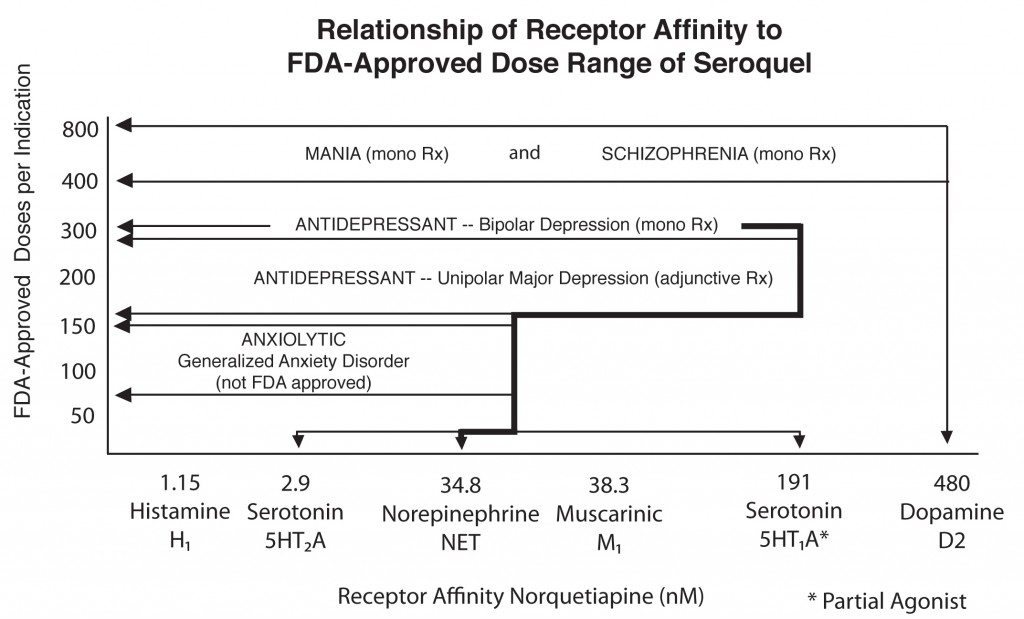
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Read more

