Nimodipine Decreases Frontal and Parietal Cortical Activity During Working Memory in Healthy Subjects
At a recent scientific meeting, researcher Kristin Bigos and colleagues described the effects of nimodipine, a treatment for brain hemorrhage, on the brain during working memory tasks. Nimodipine is a dihydropyridine L-type calcium channel blocker. Calcium channel blockers prevent calcium from entering cells in the heart and blood vessel walls, and they are often used to treat high blood pressure.
Nimodipine acts on the CACNA1C calcium influx gene. Certain genetic variations in this gene (particularly the rs1006737 A allele) have been linked to vulnerability to bipolar disorder, schizophrenia, depression, and autism. Carriers of the risk allele also have higher CACNA1C mRNA expression in the dorsolateral prefrontal cortex and exhibit more activity in the frontal and parietal regions of the brain during working memory tasks, suggesting inefficient brain processing in these regions. Bigos and colleagues found that 60mg/day of nimodipine decreased frontal and parietal cortical activity by 39.1% and 42.8%, respectively, during a working memory task, suggesting that nimodipine improved the efficiency of memory processing. Nimodipine’s positive effects were greater in those participants who had the CACNA1C risk allele.
Editor’s Note: Using a placebo-controlled off-on-off-on study design (meaning patients took placebo for a period, then nimodipine, then placebo again and nimodipine again), this editor (Robert M. Post), Peggy J. Pazzaglia and colleagues found that nimodipine had positive effects in both mania and depression in patients with bipolar disorder (described in the 2008 book Treatment of Bipolar Disorder: A Casebook for Clinicians and Patients by Robert M. Post and Gabriele S. Leverich). In a large randomized study of patients with bipolar disorder presented by Haroon R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry, lithium was associated with about a 50% response rate while the combination of lithium and nimodipine was associated with a 73% response rate.
It remains to be seen whether people with bipolar disorder who have the CACNA1C risk gene would respond better to nimodipine than those without the risk gene, and whether it would improve working memory more in the subgroup with the risk gene.
Ketamine May Enhance the Effects of Cognitive Training Therapy
Rebecca B. Price, a professor of Psychiatry and Psychology at the University of Pittsburgh, and colleagues reported at a recent scientific meeting that the combination of intravenous ketamine treatment and four days of cognitive training to enhance positive self-representations improved depression better than either intervention alone (IV ketamine plus a sham training or a non-medicated saline drip plus 4 days of cognitive work).
Price and colleagues suggested that priming brain plasticity with ketamine could enhance cognitive training focused on increasing positive self-representations. Psychologists have theorized that self-representations (or assessments of one’s strengths and other qualities) can be a resource that helps people cope with life stress.
Il-6 Inhibitor Sirukumab May Improve Anhedonia, But Not General Depression
 At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
The degree of improvement in anhedonia was significantly correlated with patients’ baseline levels of the inflammatory marker CRP. Since the inflammatory marker that sirukumab targets, Il-6, is one of those most often elevated in depression, it appears that more study of sirukumab would be warranted.
Low Levels of Acetyl-L-Carnitine Associated with Insulin Resistance in Traumatized Children
 Researcher Carla Nasca and colleagues from the Rockefeller University reported at a late-2018 scientific meeting that depressed patients with a history of childhood adversity had low levels of the amino acid acetyl-L-carnitine and also exhibited insulin resistance. This is noteworthy because in a series of small studies, acetyl-L-carnitine supplements have had antidepressant effects. In laboratory animals, acetyl-L-carnitine also sensitizes insulin receptors. This suggests the possibility that the supplements could provide a two-for-one benefit in depressed patients with a history of adversity in childhood.
Researcher Carla Nasca and colleagues from the Rockefeller University reported at a late-2018 scientific meeting that depressed patients with a history of childhood adversity had low levels of the amino acid acetyl-L-carnitine and also exhibited insulin resistance. This is noteworthy because in a series of small studies, acetyl-L-carnitine supplements have had antidepressant effects. In laboratory animals, acetyl-L-carnitine also sensitizes insulin receptors. This suggests the possibility that the supplements could provide a two-for-one benefit in depressed patients with a history of adversity in childhood.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
White Matter Abnormalities in Obesity
Researcher Ramiro Reckziegel and colleagues reported at a recent scientific meeting that white matter is abnormal in obese adults with bipolar disorder. In a 2018 article in the journal Schizophrenia Bulletin, Reckziegel reported that body mass index (BMI) was associated with reduced fractional anisotropy, a measure of brain fiber integrity, in the cingulate gyrus in patients with bipolar disorder. This finding implies that obesity may play a role in white matter microstructure damage in the limbic system.
White Matter Abnormalities Linked to Irritability in Both Bipolar Disorder and DMDD
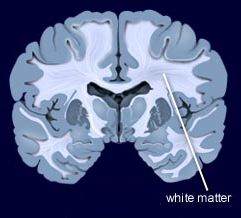 At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
At a 2018 scientific meeting, researcher Julia Linke of the National Institute of Mental Health reported that there were white matter tract abnormalities in young people who had irritability associated with either bipolar disorder or disruptive mood dysregulation disorder (DMDD). Thus, while these two disorders differ in terms of diagnosis, presentation, and family history, they seem to have this neurobiological abnormality in common.
Scientific Mechanisms of Rapid-Acting Antidepressants
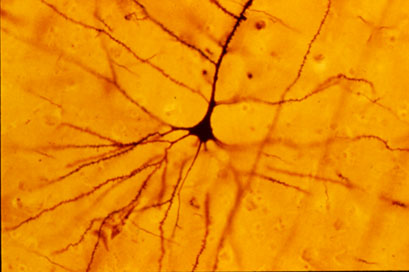
A pyramidal cell (Photo by Bob Jacobs, Laboratory of Quantitative Neuromorphology Department of Psychology Colorado College)
At a recent symposium, researcher Francis McMahon provided electrophysiological evidence that several different types of rapid-acting antidepressants—low-dose ketamine, scopolamine, and rapastinel (a partial agonist of the neurotransmitter NMDA)—act by decreasing the inhibitory effects of GABAergic interneurons on excitatory neurons called pyramidal cells, thus increasing synaptic firing.
Researcher Ronald Duman further dissected these effects, showing that ketamine and its active metabolite norketamine reduce the steady firing rate of GABA interneurons by blocking NMDA receptors, while the partial agonist rapastinel acts on the glutamate neurons directly, and both increase the effects of a type of glutamate receptors known as AMPA. These effects were demonstrated using a virus to selectively knock out GluN2B glutamate receptor subunits in either GABA interneurons or glutamate neurons.
Increasing AMPA activity increases synapse number and function and also increases network connectivity, which can reverse the effects of stress. Duman and colleagues further showed that when light is used to modulate pyramidal cells (a process called optogenetic stimulation) in the medial prefrontal cortex, different effects could be produced. Stimulating medial prefrontal cortex cells that contained dopamine D1 receptors, but not D2 receptors, produced rapid and sustained antidepressant effects. Conversely, inhibiting these neurons blocked the antidepressant effects of ketamine. Stimulating the terminals of these D1-containing neurons in the basolateral nucleus of the amygdala was sufficient to reproduce the antidepressant effects. These data suggest that stimulation of glutamate D1 pyramidal neurons from the medial prefrontal cortex to the basolateral nucleus of the amygdala is both necessary and sufficient to produce the antidepressant effects seen with ketamine treatment.
Researcher Hailan Hu reported that NMDA glutamate receptors drive the burst firing of lateral habenula (LHb) neurons, which make up the depressogenic or “anti-reward center” of the brain and appear to mediate anhedonic behavior (loss of interest or enjoyment) in animal models of depression. Ketamine blocks the burst firing of the LHb neurons, which disinhibits monoamine reward centers, enabling ketamine’s rapid-onset antidepressant effects. This may occur because inhibitory metabotropic glutamate receptors (mGluR-2) are activated, decreasing the release of glutamate.
MGluR-2 may also help explain the antidepressant effects of acetyl-L-carnitine supplements. L-carnitine is an amino acid that is low in the blood of depressed patients. The supplement acetyl-L-carnitine (ACL) activates the DNA promoter for mGluR-2, increasing its production and thus decreasing excess glutamate release. The acetyl group of the ACL binds to the DNA promoter for mGluR-2, thus this process seems to be epigenetic. Epigenetic mechanisms affect the structure of DNA and can be passed on to offspring even though they are not encoded in the DNA’s genetic sequence.
Risk of Suicide in People with Bipolar Disorder: Lowest with Lithium, Highest with Antidepressants
Researcher Markku Lähteenvuo and colleagues reported in the journal JAMA Psychiatry in early 2018 that long-acting injectable antipsychotics and lithium were best at preventing re-hospitalization in 18,018 bipolar patients in Finland who received an average of more than 7 years of follow up. Lähteenvuo and colleagues have now gone on to analyze suicide data from the same cohort of patients with bipolar disorder, and report that those taking lithium had the lowest rate of suicide, while those taking valproate had the next lowest suicide rate. Those patients with bipolar disorder who were treated with antidepressants had the greatest suicide rate. The suicide rate was particularly high for those once-hospitalized patients taking the MAO inhibitor antidepressant meclobemide, which is not approved for use in the US. Increased rates of suicide were also seen with use of sedatives and benzodiazepines.
Editor’s Note: Evidence continues to mount that lithium should be the definitive first line therapy in bipolar disorder for a multitude of reasons (as this editor Robert M. Post reviewed in an open-access article in the journal Neuropsychopharmacology in 2017). Still, lithium is not often prescribed for people with bipolar disorder in the US, and this does not seem to be in these patients’ best interests.
Use of antidepressants in bipolar disorder has remained controversial, but it is common in clinical practice despite a lack of evidence that it is effective, and the presence of some evidence that it is actually harmful. Antidepressant use in a person with bipolar disorder may cause switching into mania, cycle acceleration, dysphoria induction, and even suicide.
Clinicians should take these data seriously and overcome the impulse (leftover from treating unipolar depression) to use unimodal antidepressants as first line or adjunctive therapy for bipolar depression. Antidepressants are only effective in the long term in about 15% of patients with bipolar depression, and now it appears antidepressant use also carries an additional risk of suicide.