Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
Cool Head May Help Insomnia
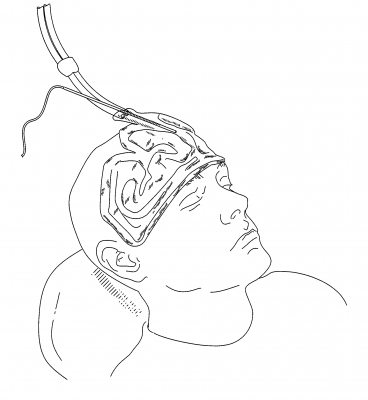
The US Food and Drug Administration recently approved a device that improves sleep by cooling the forehead. People with insomnia often have an active frontal cortex that keeps their thoughts racing as they try to fall asleep, preventing deeper, more restorative sleep. Through conducting functional brain imaging studies, researcher Eric Nofzinger found that cooling participants’ foreheads to a precise level during the night improved the quality of their sleep.
The sleep studies included more than 230 patients observed over 3800 research nights. One such study found that participants reached stage 1 and stage 2 sleep faster when they used the device.
Nofzinger founded the company Cerêve to produce the new bedside device, which pumps cooled fluid to a pad worn on the forehead. The company expects to release the device in 2017.
Insomnia may affect as many as 55 million Americans, frustrating them at night and leading to decreased alertness the following day. Sleeping pills are the most common treatment, but they can also cause impairment the following day.
Ketamine Improves Sleep and Reduces Suicidal Thoughts in Certain Patients
Intravenous ketamine is known for its fast-acting antidepressant effects, which can appear within two hours of an infusion. Researchers are now investigating its use for the reduction of suicidal thoughts. In a study presented in a poster at the 2015 meeting of the Society of Biological Psychiatry, Jennifer L. Vande Voort and colleagues compared the sleep of patients whose suicidal thoughts decreased after a single ketamine infusion (0.5 mg/kg over 40 minutes) to those whose suicidal thoughts remained.
Study participants whose suicidal thoughts diminished after one infusion of ketamine had better sleep quality the following night, with fewer disruptions in sleep than among those who did not have an anti-suicidal response to ketamine. The participants who responded well to ketamine had sleep quality similar to that of healthy controls.
Vande Voort and colleagues hope that these new findings about ketamine’s effect on sleep may provide clues to the biological mechanism behind ketamine’s effect on suicidal ideation.