Insomnia Plays Critical Role in Bipolar Disorder

In a 2021 article in the Journal of Psychiatric Research, researcher Laura Palagini and colleagues reported that insomnia symptoms can affect the course of bipolar illness. In a helpful summary and interview in the Psychiatry & Behavioral Health Learning Network’s Psych Focus, she stated that:
“1) BD patients in a depressive phase with clinically significant insomnia met a greater severity not only of depressive symptoms and suicidal risk, but also of early life stressors and the cognitive part of hopelessness, compared with patients without insomnia
“2) insomnia symptoms could predict mood symptoms, suicidal ideation and plans, and the cognitive component of hopelessness
“3) insomnia symptoms might mediate the effect of early life stressors on mood symptoms, hopelessness, and suicidal ideation and behaviors.”
Palagini suggested that “Insomnia symptoms should be easily addressed in clinical practice with 1–2 questions. Insomnia treatment should be considered as a treatment to prevent …relapse and recurrence [of bipolar disorder] and to prevent suicide and the effect of early life stress on [bipolar disorder].”
Editor’s Note: Regular nightly rating of mood, functioning, hours of sleep, medications, life events, side effects, and other comorbid symptoms on the Monthly Mood Chart Personal Calendar (pdf) is an easy way for patients with bipolar disorder to carefully track their illness trajectory and the completeness of their response to medications.
A decrease in the hours of sleep should be used as a possible early warning sign of impending difficulties, or even a new episode. Patients should discuss with their physician the threshold of insomnia (such as the loss of 2 hours of sleep for two days in a row) that should trigger a call to the physician, and what interventions the patient might initiate for lesser amounts of sleep loss and/or changes in mood. Heading these off early may prevent the breakthrough of a full-blown manic or depressive episode.
Cool Head May Help Insomnia
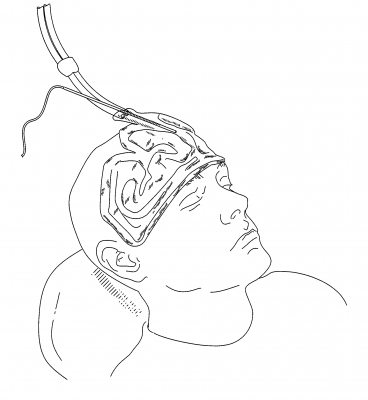
The US Food and Drug Administration recently approved a device that improves sleep by cooling the forehead. People with insomnia often have an active frontal cortex that keeps their thoughts racing as they try to fall asleep, preventing deeper, more restorative sleep. Through conducting functional brain imaging studies, researcher Eric Nofzinger found that cooling participants’ foreheads to a precise level during the night improved the quality of their sleep.
The sleep studies included more than 230 patients observed over 3800 research nights. One such study found that participants reached stage 1 and stage 2 sleep faster when they used the device.
Nofzinger founded the company Cerêve to produce the new bedside device, which pumps cooled fluid to a pad worn on the forehead. The company expects to release the device in 2017.
Insomnia may affect as many as 55 million Americans, frustrating them at night and leading to decreased alertness the following day. Sleeping pills are the most common treatment, but they can also cause impairment the following day.
Depression in Youth Is Tough to Treat and Requires Persistence and Creativity
 At a symposium on ketamine for the treatment of depression in children at the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, David Brent, a professor at the University of Pittsburg, gave the opening talk on the fact that as many as 20% of adolescents who are depressed fail to improve, develop chronic illness, and are thus in need of alternatives to traditional treatment. Predictors of non-improvement include substance use, low-level manic symptoms, poor adherence to a medication regimen, low blood levels of antidepressants, family conflict, high levels of inflammation in the body, and importantly, maternal depression. In adolescents insomnia was associated with poor response, but in younger children insomnia was associated with a better response.
At a symposium on ketamine for the treatment of depression in children at the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, David Brent, a professor at the University of Pittsburg, gave the opening talk on the fact that as many as 20% of adolescents who are depressed fail to improve, develop chronic illness, and are thus in need of alternatives to traditional treatment. Predictors of non-improvement include substance use, low-level manic symptoms, poor adherence to a medication regimen, low blood levels of antidepressants, family conflict, high levels of inflammation in the body, and importantly, maternal depression. In adolescents insomnia was associated with poor response, but in younger children insomnia was associated with a better response.
Brent suggested using melatonin and sleep-focused cognitive behavioral therapy for insomnia in youth, but not using trazodone (which is commonly prescribed). Trazodone is converted to a compound called Meta-chlorophenylpiperazine or MCPP, which induces anxiety and dysphoria. MCPP is metabolized by hepatic enzymes 2D6, and fluoxetine and paroxetine inhibit 2D6, so if trazodone is combined with these antidepressants, the patient may get too much MCPP.
Surprisingly and contrary to some data in adults about the positive effects of therapy in those with abuse histories, in the study TORDIA (Treatment of SSRI-Resistant Depression in Adolescents), if youth with depression had experienced abuse in childhood, they did less well on the combination of cognitive behavioral therapy and selective serotonin reuptake inhibitors (SSRIs) compared to SSRIs alone.
New Drug for Insomnia
The Federal Drug Administration (FDA) review committee suggested that a new type of drug for the treatment of insomnia might be approved in the future if the company who produces the drug, Merck, begins manufacturing it in smaller doses.
The drug, suvorexant, works differently from most sleep medications. Instead of creating sleepiness, it blocks a type of neurotransmitters called orexins, which are responsible for wakefulness. (Suvorexant is a selective antagonist of orexin receptors OX1R and OX2R and blocks the binding of orexin A and B to these receptors, presumably inhibiting activation of neurons of the arousal system.) The drug has a 12-hour half-life, longer than other insomnia drugs, thus morning carryover sedation is a potential problem.
The FDA asked that suvorexant be produced at the lower dose of 10mg, with the option of prescribing it at higher doses (15mg to 20mg) if a patient tolerated the 10mg dose and that dose did not sufficiently improve the patient’s insomnia. Merck had initially proposed doses of 15mg to 40mg.
Ambien Linked to Emergency Room Visits, Among Other Risks
Zolpidem, better known by one of its trade names, Ambien, is widely prescribed for the short-term treatment of insomnia. It can sometimes cause adverse reactions, particularly among women and the elderly. The Substance Abuse and Mental Health Services Administration (SAMHSA) has reported that over a recent 5-year period, emergency department visits for adverse reactions to zolpidem increased by almost 220%.
Peter Delaney, Director of SAMSHA’s Center for Behavioral Health Statistics and Quality, suggested that doctors should consider alternative strategies for treating insomnia, including improving sleep hygiene by avoiding caffeine, exercising regularly, and sleeping in a quiet, dark room. He also suggested that doctors should be aware of what other medications a patient is taking, and ideally all of a patient’s prescriptions should be collected from the same pharmacy, so the pharmacist can act as a second pair of eyes identifying possible drug interactions.
Women and men metabolize zolpidem differently, and according to Sam Fleishman of the American Academy of Sleep Medicine, many women can still be impaired by the drug 8 hours after taking it. In 2013, after reports of adverse reactions to zolpidem increased, the Federal Drug Administration (FDA) required manufacturers of drugs containing zolpidem to reduce the recommended dose for women by half, from 10 mg to 5 mg, or 12.5 mg to 6.25 mg for the extended-release version. The FDA also suggested halving the dosage prescribed to the elderly, and reducing the recommended dose for men.
Some of the adverse reactions to drugs containing zolpidem include daytime drowsiness, dizziness, hallucinations, sleepwalking, and even “sleep driving.” When combined with antianxiety medications, narcotic pain relievers, or alcohol, zolpidem’s sedative effects can be enhanced to dangerous levels.
Treating Generalized Anxiety Disorder
Generalized anxiety disorder (GAD) is a prevalent illness often associated with considerable discomfort and dysfunction. It often co-occurs with bipolar disorder. Traditional treatments of the primary syndrome (occurring in the absence of bipolar disorder) involve serotonin-selective antidepressants and serotonin-noradrenergic reuptake inhibitors such as venlafaxine (Effexor) or duloxitine (Cymbalta). While these are often useful and lead to considerable improvement, they often do not lead to full remission of somatic or accompanying symptoms of insomnia.
Alternative treatment possibilities include the anticonvulsant pregabalin (Lyrica), which has been found effective in four placebo-controlled studies in GAD. A poster presentation by Joshi et al. at the American Psychiatric Association meeting in San Francisco in May 2009 also reported that pregabalin was more effective in reducing sleep disturbance than venlafaxine. Pregabaline is FDA-approved for seizures and fibromyalgia, but not for GAD or pain syndromes. Another treatment possibility is quetiapine (Seroquel), where not only have there been positive efficacy in placebo-controlled studies of patients with GAD, but the patients also experienced improvement in sleep.
Read more