Adiposity and Cognitive Function Are Bidirectionally Related
Sakib et al reported in JAMA New Open that ” In this cohort study that included 11,103 adolescents, executive function and episodic memory were bidirectionally associated with adiposity, and this association was statistically mediated through the morphology of the lateral prefrontal cortex. Obesity (BMI) was associated worse executive functioning, episodic memory, and task performance. Thus preserving cognition is another reason beyond physical health to follow a good diet, get exercise, and use medications for weight loss if obesity is a problem.”
Cognitive Abnormalities in Patients Recently Diagnosed with Bipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Kamilla Miskowiak described a study in which she and her colleagues grouped 158 patients in remission from recently diagnosed bipolar disorder into groups based on their neurocognitive functioning and particularly their emotional processing, and also observed cognitive function in 52 first-degree relatives of those with bipolar disorder. These groups were compared to 110 healthy control participants.
Miskowiak and colleagues identified three clusters among the patients with bipolar disorder: 23% were globally impaired, 31% were selectively impaired, and 46% had normal cognition. Those who were globally impaired had problems recognizing facial expressions in social scenarios. Cognitive impairment has previously been documented in patients who have had a longer duration or more episodes of bipolar illness.
First-degree relatives of cognitively impaired patients had impaired recognition of facial expressions, but their cognition in non-emotional areas was normal. Miskowiak and colleagues concluded that the impaired affective cognition in relatives of patients with neurocognitive impairment was an indication of inherited risk for bipolar disorder.
Editor’s Note: Children with bipolar disorder also have this deficit in facial emotion recognition. That 23% of recently diagnosed patients with bipolar disorder were globally impaired indicates that some cognitive impairments can emerge early in the course of bipolar disorder. Researcher Lakshmi Yatham has previously found that cognition improves after a first episode of mania only if no further episodes occur in the one year following, indicating that episode prevention is crucial even after a patient’s first episode.
In Animal Model, Long-Term THC Exposure Interferes with Cortical Control of the Nucleus Accumbens

In an article in the journal Biological Psychiatry, researchers Eun-Kyung Hwang and Carl R. Lupica reported that in rats, long-term use of THC (tetrahydrocannabinol) weakens input from the cortex to the reward area of the brain, the nucleus accumbens (NAc). Long-term THC use also strengthens connections to the NAc from emotional control (limbic) regions, such as the basolateral amygdala and ventral hippocampus. Hwang and Lupica reason that this shift from cortical control of the NAc to limbic control likely contributes to the cognitive and psychiatric symptoms associated with cannabis use.
Editor’s Note: Street marijuana largely contains THC rather than CBD, the beneficial, anxiety-reducing component of cannabis. Cannabis products are being decriminalized, but it is important to remember that those with THC are linked to cannabis use disorder and increased susceptibility to psychiatric illness. Patients with bipolar disorder who use marijuana also have a more adverse course of illness than those who do not use it.
Treating Symptoms of Bipolar Disorder in Children at Risk
At the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, one symposium was devoted to new research on predicting onset of bipolar disorder in children who have a family history of the disorder. Below are some of the findings that were reported. See previous articles for more on this symposium.
Sub-Threshold Bipolar Disorder or BP-NOS is Impairing and Requires Treatment
In research Danella M. Hafeman’s research, children with BP-NOS were almost as ill as those with bipolar I disorder (BP I) and experienced equal incidence of suicide attempts, substance abuse, other simultaneous psychiatric diagnoses, and functional impairment, clearly indicating that they were in need of treatment. About 50–65% of participants with a family history of bipolar disorder converted from diagnoses of BP-NOS to BP I, while those with BP-NOS and no family history of bipolar disorder converted to BP I at rates of about 30–48%.
Several presenters presented data showing that those with sub-threshold bipolar disorder had severe functional impairment, a high incidence of suicide attempts, and additional diagnoses including ADHD, conduct disorder, anxiety, and substance abuse.
Diagnostic Tool Can Help Identify Children with Bipolar Disorder
Researcher Amy Yule indicated that a tool called the Child Behavior Checklist (CBCL) is effective for making the diagnosis of conduct disorder in children with bipolar disorder, while researcher Joseph Biederman showed that the CBCL can also identify children with bipolar I disorder and is faster and simpler to use in clinical practice than are full structured diagnostic interviews.
Researcher Janet Wozniak found that there was a high incidence of bipolar disorder in first-degree relatives of children with sub-threshold bipolar disorder, suggesting the validity of identifying youth with sub-threshold bipolar symptoms.
As discussed above, there is also a high incidence of children with BP-NOS progressing to a full diagnosis of bipolar I or II disorder (as many as 50% of those with a family history of bipolar disorder). However, the point is not to wait for the negative effects of a full diagnosis before beginning treatment: BP-NOS itself requires treatment.
Discussion and Emerging Consensus on Treatment, Particularly of BP-NOS
Experts in the field agree that family focused therapy (FFT) or its equivalent is a crucial first step to treatment of depression, cyclothymia (cycling between depressive and hypomanic symptoms that do not meet the threshold for a diagnosis of bipolar disorder), and BP-NOS in children who are at high risk of bipolar disorder because they have a parent with the disorder.
A second area of agreement is that young people with BP-NOS should have a positive therapeutic coach (which could be a treating physician if no other person is available), who can emphasize important early steps that can improve short- and long-term health. These include maintaining a healthy diet, exercise (such as participation in school sports), the practice of mindfulness and/or meditation, and playing and practicing a musical instrument. Parental support is also critical to decreasing negative expressed emotion.
Early interventions and wellness programs that focus on these factors are part of the successful Vermont Family Based Approach, led by psychiatrist Jim Hudziak, Director of the Vermont Center for Children, Youth, and Families. Since programs like these are not widely available, treating physicians must create their own teams to provide such encouragement, and teach families how to find or establish such a support network.
School teachers should be engaged in support of the treatment of a child with bipolar disorder. Teachers should pay special attention to behavioral symptoms of an ill child. It also may be important for physicians to connect directly with teachers to ensure that children recovering from an episode of bipolar disorder receive extra time for assignments, a decreased academic burden, and other support. Researcher Manon H. Hillegers indicated that intervention by a physician will likely be listened to and believed, while parental requests alone to teachers or to the school may go ignored.
Hillegers, like researcher Lakshmi Yatham and colleagues, have found that it takes a year after a first manic episode for a child’s cognition to return to normal, so that special allowances should be made for such students even many months after they have recovered from their mania.
Positive Effects of a Brief Session of Aerobic Exercise for Sedentary Children
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Benjamin I. Goldstein reported that a single 20-minute session of aerobic exercise (achieving 70% of maximal heart rate) was associated with improvement in cognition and in abnormalities seen on brain imaging in young people. Goldstein urged clinicians to do motivational interviews with sedentary children in their care, emphasizing the positive cardiovascular and cognitive effects of exercise. He indicated this would be more effective than a focus only on weight loss, which is much more difficult to achieve.
Inflammation Associated with Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Katherine E. Burdick and colleagues at Brigham and Women’s Hospital and Harvard Medical School reported that in 240 patients with bipolar disorder who were not currently having a manic or depressive episode, markers of inflammation were associated with cognitive deficits.
Inflammation was associated with cognitive deficits in general, and there were also some relationships between specific inflammatory markers and types of cognitive processing. They found that the inflammatory markers TNF-alpha, TNFR1, and TNFR2 influenced cognitive flexibility. The inflammatory marker VEGF influenced reward processing, while IL-6/IL-6r influenced spatial processing. IL-1beta and IL-1RA influenced social cognition.
Burdick and colleagues found it was important to include both primary and secondary mediators of inflammation in their research “as the effects of the primary pro-inflammatory cytokines can be blocked by a number of decoy receptors and soluble antagonists.” Elevations in these can provide additional information about the function of the immune system.
Editor’s Note: Targeting inflammation with the anti-inflammatory treatments minocycline and celecoxib has been shown to improve depression. Now the role of anti-inflammatory drugs in improving cognition deserves further attention.
Links Between Mixed Depression, Insulin Resistance, Inflammation, and Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre discussed links between obesity, diabetes, and cardiovascular problems; increased inflammation; and decreased functioning of the neural networks involved in cognition.
He and his colleagues analyzed 121 studies that included empirical research and meta-analyses. McIntyre and colleagues found that patients with higher levels of inflammatory markers have more insulin resistance and cognitive dysfunction. A meta-analysis revealed that the inflammatory markers IL-6, TNF alpha, and CRP were significantly elevated in people with bipolar disorder compared to normal controls, while IL-1B was not.
People with depression who had a few manic traits (mixed depression) were particularly likely to have insulin resistance and elevated levels of pro-inflammatory markers.
People with mixed depression have increases in inflammation and increased incidence of cardiovascular disorder. People experiencing a first episode of mixed depression who are overweight show increased signs of brain aging.
In studies McIntyre and colleagues analyzed, diabetes or pre-diabetes occurred in 50% of depressed patients, and these patients had the greatest amount of cognitive dysfunction.
Treatment
McIntyre noted that taking the antipsychotic drug lurasidone for bipolar depression worked best in both adults and children who had elevated levels of CRP at baseline. The fast-acting antidepressant ketamine also works well in those who show baseline inflammation .
The anti-diabetes drug liraglutide (Victoza, Saxenda) improves mixed depression symptoms and cognition in obesity, diabetes, and mixed depression. Liraglutide belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists or incretin mimetics. They work by increasing insulin release from the pancreas and decreasing excessive glucagon release.
McIntyre now routinely uses liraglutide for cognitive deficits in patients with obesity or diabetes, including patients with mixed depression. It is injected under the skin at 0.6 mg daily, then the dosage is increased to 1.2 mg and then 1.8 mg. Victoza reduces major cardiovascular events in those with type 2 diabetes. The higher-dose Saxenda (3mg) can be used for weight control.
Another anti-diabetes drug, pioglitazine, has also been reported to be helpful in bipolar depression.
McIntyre found that the antibody infliximab, which can be used as an intravenous treatment for chronic inflammation and works by blocking the effects of TNF-alpha, did not improve depression, but did improve cognition.
McIntyre also supports the use of acetyl-L-carnitine, a potential adjunctive treatment that can reverse the insulin resistance that often occurs with obesity and thus could theoretically improve cognition.
McIntyre described preliminary literature suggesting the effectiveness of drugs such as statins, calcium channel blockers, and biguanides such as the diabetes treatment metformin in reducing inflammation.
Bariatric surgery to reduce the size of the stomach was another option discussed by McIntyre. He said the intervention is safe for patients with bipolar disorder and can help them recover cognitive function.
McIntyre noted that offspring of a mother with obesity have decreased response to sensory cues, reward preference, cognitive control, and motor control. Obesity and the inflammation that goes along with it apparently affect offspring via epigenetic mechanisms, meaning obesity may change the structure of inherited DNA (without changing its sequence).
Vitamin D3 Improves Depression in Older Adults
Researcher Negin Masoudi Alavi and colleagues reported in the journal Clinical Nutrition in 2018 that compared to placebo, 50,000 IU of vitamin D3 taken weekly for eight weeks improved depression in depressed patients over the age of 60.
Although the literature about vitamin D3’s effects on depression are mixed, a 2014 meta-analysis by Simon Spedding in the journal Nutrients found that in studies of vitamin D-deficient depressed participants whose vitamin D levels were restored to normal levels by the end of the study, vitamin D significantly improved depression. (Spedding attributed earlier mixed results to studies that did not clearly correct a vitamin D deficiency.) A 2013 study by Nayereh Khoraminya and colleagues in the Australian and New Zealand Journal of Psychiatry suggested that a 1500 IU dose of vitamin D3 combined with the selective serotonin reuptake inhibitor (SSRI) antidepressant fluoxetine improved depression more than fluoxetine plus placebo in depressed patients who were not necessarily deficient in vitamin D. Another study by Jacqueline A. Pettersen in the journal Experimental Gerontology found that in healthy adults, 4,000 IU of vitamin D3 improved cognitive functioning (namely visual memory) more than 400 IU.
Editor’s Note: Given these promising studies, the safety of D3, and fact that psychiatric patients are often deficient in vitamin D3, taking vitamin D3 supplements to improve depression might be worth trying.
Using Light to Improve Sleep and Depression
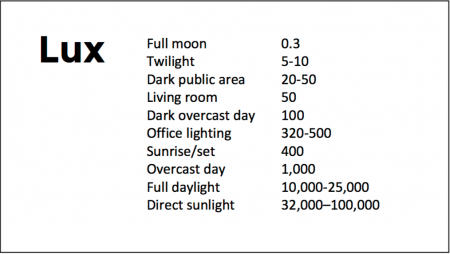
At the 2018 meeting of the North Carolina Psychiatric Association, researcher Chris Aiken described the phenomenon of sleep inertia, when people are awakened from deep sleep by an alarm, rather than waking at the end of a sleep cycle, and are groggy for 15 minutes. Depressed people may stay groggy for 4 hours. A dawn simulator may help. These lights turn on gradually over the course of 30 to 60 minutes, reaching 250 lux while the patient is still asleep. Dawn simulators have worked in eight out of ten controlled clinical trials to help people with seasonal affective disorder, adolescents, and normal adults wake up more easily. They range in cost from $25 to $90 and some brands include PER2LED or LightenUp. Aiken says dawn simulators can improve depression, sleep quality, and cognition.
Evening and nighttime light: Bright lights and blue light, like the light that comes from electronic screens, can shut down the body’s secretion of melatonin, making people awake and alert in the evening when they should be getting sleepy. Dim light or glasses that filter out blue light allow increases in melatonin secretion in the evening, while bright light suppresses it. Missing this early melatonin pulse creates “night owls” who have delayed sleep onset.
Because light still reaches our eyes through our eyelids as we sleep, even low-level light during the night impairs sleep, cognition, and learning, and increases the risk of depression by a hazard ratio of 1.8 (about double the risk). A 2017 study by Kenji Obayashi in the American Journal of Epidemiology found that bedroom light above 5 lux elevated rates of depression in older adults after two years of followup. Living room light averaged around 50 lux and increased depression further.
The treatment is turning off TVs, electronic screens, and cellphones in the evening or wearing blue-blocking glasses, which can be found for less than $10. Blue-blocking glasses can increase calmness and reduce anxiety, and even are effective in treating mania. Then, during sleep, wear an eye mask or get light-blocking blinds or curtains for windows. For a complete blackout, use blackout curtains, aluminum foil over windows, electric tape over LED lights, or try sleeping in the basement.
Aiken suggests that to re-instate healthy sleep patterns, people should institute virtual darkness from 6pm to 8am, including wearing blue-blocking glasses when out of bed. Then they should institute total darkness or wear an eye mask when in bed. When symptoms improve, this routine can gradually be shifted to begin later in the evening, such as two hours before bedtime.
Blue light filters are also available for smartphones and tablets including Apple Nightshift mode, Kindle BlueShade, and Android Twilight and Blue Light Filter.
Glasses that filter out blue light include Uvex Ultraspec 2000, 50360X ($7 on Amazon) and Uvex Skyper 351933X ($7-10 on Amazon). The website lowbluelights.com sells blue-blocking glasses from $45 and a variety of other blue-free lighting products such as lightbulbs and flashlights.
Bright light therapy for unipolar and bipolar depression: 30 minutes of bright light (7,500 to 10,000 lux) in the morning can help treat depression in unipolar and bipolar disorder and seasonal affective disorder. The effects usually take 3 to 7 days to set in, but they only last while a patient continues using the bright light in the morning. Researcher Dorothy K. Sit and colleagues found that bright light therapy in the morning sometimes caused hypomanic reactions in people with bipolar disorder, and reported in a 2018 article in the American Journal of Psychiatry that midday light therapy (from noon to 2:30pm) was also effective without this unwanted effect. However, a 2018 article by Ne?e Yorguner Küpeli and colleagues in the journal Psychiatry Research suggested that a half hour of morning light for two weeks was sufficient to bring about improvement in 81% of patients with bipolar disorder and did not cause serious side effects.
Melatonin regimen for sleep onset delay: Melatonin can be used to treat severe night-owls with a very late onset of sleep (for example, going to bed at 2 or 3am and sleeping late into the morning). Melatonin can help with sleep onset to some extent when used at bedtime, but in those with an extreme phase shift, researcher Alfred J. Lewy recommends a regimen of low dose priming with 400–500 micrograms of melatonin at 4pm and then a full dose of 3 milligrams of melatonin at midnight. The 4pm priming dose helps pull back the delayed onset of the body’s secretion of melatonin toward a more normal schedule.
Grape Extract May Improve Cognition
 Polyphenolic compounds in colored fruits and vegetables are thought to improve memory and cognition. Extracts from Vitis vinifera, the grape species that includes almost all well-known varieties of wine, have been found to have many beneficial effects: antioxidant, antibacterial, anti-inflammatory, anticancer, antidiabetic effects, in addition to protective effects on skin, the heart, the liver, and neurons.
Polyphenolic compounds in colored fruits and vegetables are thought to improve memory and cognition. Extracts from Vitis vinifera, the grape species that includes almost all well-known varieties of wine, have been found to have many beneficial effects: antioxidant, antibacterial, anti-inflammatory, anticancer, antidiabetic effects, in addition to protective effects on skin, the heart, the liver, and neurons.
For about a decade, researchers have known that polyphenolic compounds from grapes could improve cognitive impairment and reduce neuropathological lesions in the brain in animals with a model of Alzheimer’s disease. New research suggests that the same compounds that protect the plant against damage, fungus, or UV rays may also protect the human brain against damage.
Researchers led by Gioacchino Calapai tested a trademarked nutritional supplement called Cognigrape, which includes extracts from Vitis vinifera, in healthy adults between the ages of 55 and 75 in Italy. One group of 57 participants received 250mg of Cognigrape per day while the other group of 54 received placebo once a day for twelve weeks. Several weeks after the supplementation period, the group taking Cognigrape showed significant improvement in cognitive function compared to baseline and compared to the group taking placebo. The Cognigrape group also showed significant reductions in depression symptoms, improvements in somatic symptoms, and improvements in attention, language, immediate memory, and delayed memory. This is the first study to find an improvement in cognitive performance in humans after supplementation with a Vitis vinifera extract.
The study by Calapai and colleagues was published in the journal Frontiers in Pharmacology in 2017.