Pediatric Bipolar Disorder is Associated with Neurocognitive Deficits
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Maria Paula Maziero of The University of Texas Health Science Center At Houston reported that while euthymic youths with BD (bipolar disorder) exhibited significant dysfunction in working memory (WM), verbal learning, and memory domains, fluctuation between the mood states affected the type of cognitive dysfunction. They concluded: “Pediatric bipolar disorder patients have marked cognitive dysfunction involving multiple domains, especially executive measures. The severity of mood symptoms influences cognitive performance, but even euthymic persons perform lower than matched controls.“
The Systematic Treatment Optimization Program for Early Mania
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
A. Rathseesh and L. Yatham reported on the importance of systematic vigorous treatment of a first manic episode. If more episodes occurred, losses in cognition did not fully recover. All patients remitted within 1 year of their first mania. Recurrence occurred in 58% by year 1 and 74% by year 4. Predictors of functional recovery included sustained euthymia, especially absence of depressive symptoms, good cognitive functioning, and maintaining a normal weight. More aggressive treatment to prevent relapses in years 1-4 after a first manic episode appears needed and how exactly to achieve this requires further study.
7-Year-Olds At Risk for Schizophrenia, But Not Bipolar Disorder, Show Specific Types of Cognitive Dysfunction
 A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
The researchers identified 7-year-olds,197 who had family members with schizophrenia, 118 who had family members with bipolar disorder, and 199 control 7-year-olds with no family history of these illnesses. Those children at risk for schizophrenia had significantly more cognitive deficits and behavioral disorders than the controls, while those children at risk for bipolar disorder did not differ significantly from the controls. The deficits among the children at risk for schizophrenia were in the areas of processing speed and working memory, executive and visuospatial functions, and declarative memory and attention.
The researchers indicated that the neurocognitive profile seen in the children at risk for schizophrenia could help clinicians identify these children for early intervention.
Inflammation Associated with Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Katherine E. Burdick and colleagues at Brigham and Women’s Hospital and Harvard Medical School reported that in 240 patients with bipolar disorder who were not currently having a manic or depressive episode, markers of inflammation were associated with cognitive deficits.
Inflammation was associated with cognitive deficits in general, and there were also some relationships between specific inflammatory markers and types of cognitive processing. They found that the inflammatory markers TNF-alpha, TNFR1, and TNFR2 influenced cognitive flexibility. The inflammatory marker VEGF influenced reward processing, while IL-6/IL-6r influenced spatial processing. IL-1beta and IL-1RA influenced social cognition.
Burdick and colleagues found it was important to include both primary and secondary mediators of inflammation in their research “as the effects of the primary pro-inflammatory cytokines can be blocked by a number of decoy receptors and soluble antagonists.” Elevations in these can provide additional information about the function of the immune system.
Editor’s Note: Targeting inflammation with the anti-inflammatory treatments minocycline and celecoxib has been shown to improve depression. Now the role of anti-inflammatory drugs in improving cognition deserves further attention.
Galantamine Did Not Improve Cognitive Deficits in People with Bipolar Disorder
In a recent study by researcher Dan V. Iosifescu and colleagues, the drug galantamine, which is used to treat dementia, did not improve cognitive function in euthymic people with bipolar disorder. The drug had done so in earlier studies. Seventy-two participants with bipolar disorder that was in remission were randomized to receive either a placebo or galantamine extended release for a period of two weeks. Doses of galantamine ranged from 8 to 24 mg/day.
The participants took several tests of attention and memory over the course of the study. After 16 weeks of treatment, those taking galantamine did not show significant improvements in functioning compared to those who received placebo.
This research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Low Vitamin D Linked to Cognitive Decline
Low levels of vitamin D levels are common, particularly in older adults and in African Americans and Hispanics. Unfortunately, low vitamin D is associated with decline in two types of cognitive functioning: episodic memory (memories of autobiographical events) and executive function (reasoning, problem-solving, planning, etc.).
A recent study with a particularly diverse group of participants, over half of whom were African American or Hispanic, found that over a period of about 5 years, episodic memory and executive function declined faster in older adults with low levels of vitamin D.
Average vitamin D levels for the entire group of 382 adults were below national standards. Levels of 25-hydroxy vitamin D should be between 20 and 50 nanograms per milliliter of blood. The average fell just below this, at 19.2 ng/mL. Over a quarter of participants had vitamin D deficiency, with levels below 12 ng/mL, and another 35.1% had vitamin D insufficiency, with levels between 12 and 20 ng/mL.
African Americans and Hispanics had lower levels of vitamin D (17.9 ng/mL and 17.2 ng/mL, respectively) than whites (21.7 ng/mL). Average vitamin D levels were lower in participants with dementia compared with those who had mild cognitive impairment or normal cognitive function.
Vitamin D levels can depend on factors such as dairy intake, sun exposure, and exercise. It has not been determined whether taking vitamin D supplements could slow down cognitive decline, but vitamin D supplementation has several benefits. Compared to placebo, supplementation with vitamin D increases response to antidepressants. A high percentage of children with major psychiatric disorders are vitamin D deficient, and it is also estimated that about 40% of adults in the US have a vitamin D deficiency.
The study by researcher Joshua W. Miller and colleagues was published in the journal JAMA Neurology in September.
Medicinal Herb May Help Cognitive Dysfunction in Bipolar Disorder
Many patients with bipolar disorder experience cognitive deficits that impede their recovery and that persist during times of wellness. In a double-blind placebo-controlled study by K. N. Roy Chengappa et al. published in the Journal of Clinical Psychiatry in 2013, the herb Withania somnifera (WSE, commonly called ashwagandha and sold under the name Sensoril) was significantly better than placebo at improving patients’ performance on three different cognitive tasks.
In the eight-week study, 53 patients took either 500 mg of WSE or placebo in addition to their regular medications.
The herb, which has traditionally been used in Ayurvedic medicine in India as an aid to resisting stress and disease, improved performance on digit span backwards (a test of short-term memory in which the subject must repeat a sequence of numbers backwards), Flanker neutral (a test of response time in which a subject must repress their instinct to give an incorrect response), and the Penn Emotional Acuity Test (which requires subjects to correctly identify facial emotions depicted in photographs).
Mood and anxiety levels were not different for the group taking WSE and the group taking placebo.
The researchers hope to continue their investigation of WSE with larger and longer-term studies that will explore the effects of different doses of WSE.
Malnutrition Early in Life Has Lasting Effects
Severe malnutrition in the first year of life even when corrected for the rest of a person’s life leaves a legacy of permanent cognitive deficits, marked deficits in attention, and increases in depression, conduct disorders, and medical disorders compared to carefully matched controls. Jamina Galler, a researcher at Harvard Medical School, gave a plenary talk at the 2013 meeting of the American Academy of Child and Adolescent Psychiatry on the long-term effects of even short-term childhood malnutrition, including marasmus (calorie deficiency) and kwashiorkor (protein deficiency).
Galler’s studies followed three generations of people born in Barbados and observed the consequences of prior malnutrition, which was completely eliminated in Barbados by 1980. The consequences of malnutrition in the first year of life not only affected the first (G1) generation, but subsequently their offspring in the G2 generation who also suffered an excess of attention-deficit hyperactivity disorder, low IQ, and low annual income into adulthood. That is, the early malnutrition had transgenerational effects.
Malnutrition is a huge problem worldwide and is especially bad in sub-Saharan Africa and some parts of Asia. Globally, malnutrition accounts for 50% of the deaths of children under age five. However, even in the US hunger is a problem for one in four children, or about 16 million individuals, and the long-term consequences of hunger remain to be further studied.
Studies in animals indicate that early malnutrition has epigenetic effects that can be passed on to four future generations before they are reversed. Epigenetic effects refer to environmental factors that cannot change the sequence of DNA, but change how easily it is transcribed by adding or taking away acetyl and methyl groups on DNA and histones, the structures around which DNA is wound. Malnutrition (defined as 6–8% casein, a type of protein, in the diet instead of the normal 25%) in rodents affects cognitive abilities and blood pressure and can lead to diabetes, obesity, and other metabolic abnormalities. The next generation is also affected because a previously malnourished mother huddles too much with her offspring, and they become obese as a result of these poor parenting skills. The second generation also exhibits epigenetic changes in the prefrontal cortex (such as too few glucocorticoid receptors due to methylation of the glucocorticoid promoter) and fewer neurons in the hippocampus.
Editor’s Note: Other data indicate similar long-lasting epigenetic and transgenerational effects of other types of childhood adversity, such as verbal, physical, or sexual abuse. These findings in humans are also paralleled by findings in animals, and give strong credence to the idea that the environment can have long-lasting effects on neurobiology and behavior via epigenetic effects that can be superimposed on whatever genetic effects are inherited.
Data from this editor (Robert Post) and colleagues on verbal abuse in childhood is striking; this supposedly less severe form of abuse is still associated with a more difficult course of bipolar disorder and an increase in medical comorbidities. Thus, the experience of early abuse, even just verbal abuse, appears to have long-lasting consequences for psychiatric and medical health into adulthood.
RTMS Improves Working Memory In Patients With Schizophrenia
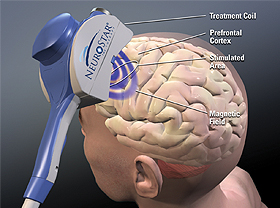 Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Repetitive transcranial magnetic stimulation (rTMS) may improve working memory in patients with schizophrenia, according to a small study published by Zafiris J. Daskalakis and colleagues in Biological Psychiatry in 2013. Patients with schizophrenia received either 20 Hz rTMS over the left and right prefrontal cortex or a sham treatment, and the rTMS improved working memory on a particular task, the n-back task, wherein patients are asked to recall whether a stimulus they’re currently viewing is the same as the previous one they viewed, or one they viewed several times back. Twenty sessions of rTMS over a period of 4 weeks brought memory back to the levels seen in normal controls.
Editor’s Note: Since many patients with bipolar disorder also have deficits in prefrontal-based memory and performance even when euthymic, it will be important to see if rTMS would also be helpful in these patients. RTMS at 20 Hz increases neuronal activity as measured by PET scan of the prefrontal cortex and other regions of the brain, and this lasts for at least 48 hours after each treatment.
Since many patients with schizophrenia and bipolar disorder show deficits in prefrontal activity at baseline, the normalization of these alterations could relate to the memory improvement. This proposition could be tested relatively easily.
White Matter Abnormalities in the Brain Predict Onset of Psychosis
 At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
Bearden found that the degree of white matter abnormality seen during magnetic resonance imaging (MRI) was proportional to the degree of cognitive deficit in patients who subsequently developed a first episode of psychosis. The white matter abnormalities were seen particularly in the superior longitudinal fasciculus (SLF) and were associated with increased severity of symptomatology. The overall degree of white matter alteration was also significantly related to clinical outcome 15 months later.
Editor’s Note: The SLF is a major neuronal conduit between prefrontal cortical systems, which are responsible for cognition and planning, and the parietal cortex, which is responsible for spatial abilities. Disruption of this fiber track has been related to difficulties in social cognition and “theory of mind” concepts, like inferring what others might be thinking.






