Psychiatric Medications Just as Effective as Medications for Other Illnesses
The popular media has sometimes scrutinized research on psychiatric medications, suggesting that they are not as effective as pharmaceutical companies would have us believe. Researchers in Germany recently performed a meta-analysis of research on psychiatric medications and found that the effect sizes for psychiatric drugs were comparable to effect sizes of other types of drugs. (Effect sizes communicate the size of the change that a drug brings about in patients.) The study was published in the British Journal of Psychiatry.
From the abstract:
Any comparison of different outcomes in different diseases can only serve the purpose of a qualitative perspective. The increment of improvement by drug over placebo must be viewed in the context of the disease’s seriousness, suffering induced, natural course, duration, outcomes, adverse events and societal values.
Antidepressants Work Better in Major Depressive Disorder than Previously Thought
As we’ve written before, the popular media has sometimes questioned the efficacy of antidepressants for unipolar depression. A reanalysis of data from previous controlled trials of fluoxetine and venlafaxine that was recently published in the Archives of General Psychiatry provides new evidence that these drugs are significantly more efficacious than placebo in youth, adult, and geriatric populations with major depressive disorder.
The researchers concluded,
To our knowledge, this is the first research synthesis in this area to use complete longitudinal person-level data from a large set of published and unpublished studies. The results do not support previous findings that antidepressants show little benefit except for severe depression. The antidepressants fluoxetine and venlafaxine are efficacious for major depressive disorder in all age groups, although more so in youths and adults compared with geriatric patients. Baseline severity was not significantly related to degree of treatment advantage over placebo.
Possible Antidepressant Effects of Memantine
 In an 8-week study of memantine for augmentation of treatment with lamotrigine for bipolar depression, memantine’s effects were not statistically significant. However, during the first four weeks of the study, while memantine doses were slowly increased, memantine was associated with significant improvements on the Hamilton Depression Rating Scale (HDRS).
In an 8-week study of memantine for augmentation of treatment with lamotrigine for bipolar depression, memantine’s effects were not statistically significant. However, during the first four weeks of the study, while memantine doses were slowly increased, memantine was associated with significant improvements on the Hamilton Depression Rating Scale (HDRS).
From the abstract:
This proof-of-concept study failed to show a statistically significant benefit of memantine augmentation of lamotrigine for patients with BD-D over eight weeks. However, memantine had an antidepressant effect early on in the treatment while its dose was being titrated up. Larger placebo-controlled studies are needed to ascertain optimal timing and dosing for memantine augmentation of lamotrigine in BD-D.
Study Calls Into Question FDA Black Box Warning about Suicide Risk in Youth Taking Antidepressants
In 2004, the Federal Drug Administration issued a “black box warning” about increased risk of suicidal thoughts and behavior in children and adolescents taking selective serotonin reuptake inhibitors (SSRIs). See here for an overview from the National Institute of Mental Health.
An article published in the Archives of General Psychiatry earlier this year analyzed data from studies of fluoxetine and venlafaxine in youth, adults, and geriatric patients to determine if antidepressant use is linked to suicide. The drugs decreased both depressive symptoms and suicidal thoughts and behavior in adults and the geriatric population. They seemed to have no effect on suicidal thoughts or behavior in the youth.
For youths, no significant effects of treatment on suicidal thoughts and behavior were found, although depression responded to treatment. No evidence of increased suicide risk was observed in youths receiving active medication.
Weight Gain and Metabolic Risks of Antipsychotic Drugs in Children and Adolescents
 A study published in the Journal of Child and Adolescent Psychopharmacology in late 2011 reviewed the various weight and metabolic side effects of drugs like olanzapine, clozapine, risperidone, quetiapine, and aripiprazole.
A study published in the Journal of Child and Adolescent Psychopharmacology in late 2011 reviewed the various weight and metabolic side effects of drugs like olanzapine, clozapine, risperidone, quetiapine, and aripiprazole.
Across 34 published head-to-head and placebo-controlled studies in youth with psychotic and bipolar disorders, weight gain ranged from 3.8 to 16.2 kg with olanzapine (n=353), 0.9-9.5 kg with clozapine (n=97), 1.9-7.2 kg with risperidone (n=571), 2.3-6.1 kg with quetiapine (n=133), and 0-4.4 kg with aripiprazole (n=451).
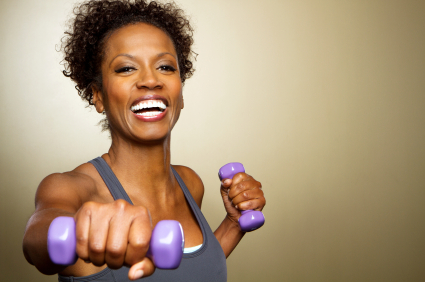
Exercise and Brain Health: Some Good Points to Remember
In a review article in the Neuroscientist published in February of this year, Kirk I. Erickson and collaborators wrote that “[m]ajor depressive disorder is considered a risk factor for Alzheimer’s dementia and memory impairment and is associated with less BDNF and greater hippocampal atrophy, possibly through a BDNF pathway. However, exercise and effective treatment for geriatric depression increases BDNF levels, increases serotonin fibers, is associated with greater hippocampal volumes, and reduces the risk for Alzheimer’s dementia.”
Editor’s note: Not a bad set of benefits from exercise! The researchers suggest that exercise is extremely important in reversing the decreases in brain-derived neurotrophic factor (BDNF) associated with depression, helping to improve depressed mood, increasing cardiovascular fitness, and maintaining healthy cognition.
Hippocampal volume and BDNF levels in blood both decrease with age. Yet exercise increases both BDNF and the formation of new neurons (neurogenesis) in animals. New data in humans suggest that aerobic fitness is associated with the size of the hippocampus, both in both children and adults. It is not clear yet whether this increase in hippocampal volume is directly driven by increases in BDNF and/or neurogenesis. However, since a smaller hippocampus is a risk factor both for depression and for mild cognitive impairment progressing to Alzheimer’s dementia, attempting to enhance hippocampal volume in any way possible is probably a good idea.
Methods of increasing hippocampal volume include treatment with antidepressants or with lithium. In the 2012 paper Erickson and collaborators also wrote, “Anaerobic exercise enhances executive and memory function and reduces hippocampal atrophy in late adulthood, and this may be partially mediated through a BDNF pathway.”
Erickson and collaborators conducted a longitudinal study published in 2010 that quantified the amount of physical activity subjects engaged in by calculating the total number of blocks walked per week. Individuals reporting greater amounts of physical activity at the beginning of the study had, upon examination nine years later, greater gray matter volume in several parts of the brain, including the hippocampus. This effect was “dose-dependent,” meaning that only those individuals who walked at least 72 blocks per week (roughly equivalent to 1 mile per day) had significant sparing of brain tissue nine years later. The study found increased gray matter volume in the prefrontal cortex and in the temporal lobe.
After a further follow-up of four more years, greater gray matter volume with physical activity was associated with a two-fold reduced risk of cognitive impairment. The researchers concluded that “physical activity patterns earlier in life were linked to brain volume and cognitive impairment later in life.”
There are a number of important points to remember about cognitive impairment. One is that increasing hippocampal volume and preventing its decrement with aging may help prevent age-related memory loss and potentially the rapidity at which mild cognitive impairment progresses. Read more
Keep Your Heart and Cardiovascular System Healthy
 Middle aged folks, watch your risk factors for cardiovascular disease. These include: high blood pressure, cholesterol, weight, and blood sugar (diabetes).
Middle aged folks, watch your risk factors for cardiovascular disease. These include: high blood pressure, cholesterol, weight, and blood sugar (diabetes).
According to Heartwire, an article in the New England Journal of Medicine indicates that having any of these risk factors increases the likelihood of cardiovascular disease later in life. The more risk factors one has, the greater the increase in risk.
Across the whole meta-analysis, participants with no risk factors at age 55 (total cholesterol level: <180 mg/dL;
blood pressure: <120 mm Hg systolic and 80 mm Hg diastolic; nonsmoking; nondiabetic) had drastically better odds
of avoiding death from cardiovascular disease through the age of 80 than participants with two or more major risk
factors (4.7% vs 29.6% among men and 6.4% vs 20.5% among women).People with an optimal risk-factor profile also had lower lifetime risks of fatal coronary heart disease or nonfatal MI (Editor’s Note: myocardial infarction, or heart attack) (3.6% vs 37.5% among men, <1% vs 18.3% among women) and fatal or nonfatal stroke (2.3% vs 8.3% among men,
5.3% vs 10.7% among women), compared with those with two or more risk factors.
What this article does not mention is that depression is a risk factor for coronary artery disease, and should be treated just as aggressively and persistently as the other cardiovascular risk factors.
Also as we’ve written before in the BNN, exercise is one element of a healthy life style that can positively affect all of these risk factors. Starting a healthy diet and exercise regimen in middle age will have long-term positive effects and reduce risks later in life.
Parental Nurturing Linked to Greater Hippocampal Volume in Young Children
An article published by Medscape reports that in a recent study by Dr. Joan Luby of Washington University School of Medicine in St. Louis, non-depressed preschool children whose parents showed more nurturing behaviors during a mildly stressful task were found to have hippocampal volume almost 10% greater than their peers whose parents showed fewer nurturing behaviors. The hippocampus affects cognitive functioning and emotion regulation.
Unfortunately, parental nurturing did not effect the hippocampal volume of children with early-onset depression.
Dr. Luby and colleagues think their findings could have “profound public health implications and suggest that greater public health emphasis on early parenting could be a very fruitful social investment.”
“The finding that early parenting support, a modifiable psychosocial factor, is directly related to healthy development of a key brain region known to impact cognitive functioning and emotion regulation opens an exciting opportunity to impact the development of children in a powerful and positive fashion”.
Parent-Child Therapy Technique Could Be Useful for Depression in Very Young Children
 There are few treatments approved by the Federal Drug Administration for the treatment of depression in very small children. But a new therapeutic technique parents can use with their children is being studied.
There are few treatments approved by the Federal Drug Administration for the treatment of depression in very small children. But a new therapeutic technique parents can use with their children is being studied.
According to an article published by the Brain and Behavior Research Foundation,
Now, a novel approach called Parent Child Interaction Therapy-Emotion Development (PCIT-ED), being tested by Brain & Behavior Research Foundation Independent Investigator Grantee Joan Luby, M.D., and colleagues at Washington University in St. Louis, has shown promise in an early trial of improving mood and behavior in very young children with depression. The results of the pilot study were reported online on Oct. 31, 2011 in the Journal of Child Psychology and Psychiatry.
PCIT-ED is a dyadic psychosocial intervention with two components. The PCIT part is aimed at strengthening the parent-child relationship by teaching positive play techniques and training parents in ways to handle children’s noncompliant and disruptive behavior. PCIT has previously been shown to be effective for treating disruptive disorders among preschoolers. The new ED component was designed to help parents enhance their children’s ability to recognize their own emotions as well as emotions in others and to more effectively regulate intense emotions.
[Editor’s Note.: our emphasis]