Grape Extract May Improve Cognition
 Polyphenolic compounds in colored fruits and vegetables are thought to improve memory and cognition. Extracts from Vitis vinifera, the grape species that includes almost all well-known varieties of wine, have been found to have many beneficial effects: antioxidant, antibacterial, anti-inflammatory, anticancer, antidiabetic effects, in addition to protective effects on skin, the heart, the liver, and neurons.
Polyphenolic compounds in colored fruits and vegetables are thought to improve memory and cognition. Extracts from Vitis vinifera, the grape species that includes almost all well-known varieties of wine, have been found to have many beneficial effects: antioxidant, antibacterial, anti-inflammatory, anticancer, antidiabetic effects, in addition to protective effects on skin, the heart, the liver, and neurons.
For about a decade, researchers have known that polyphenolic compounds from grapes could improve cognitive impairment and reduce neuropathological lesions in the brain in animals with a model of Alzheimer’s disease. New research suggests that the same compounds that protect the plant against damage, fungus, or UV rays may also protect the human brain against damage.
Researchers led by Gioacchino Calapai tested a trademarked nutritional supplement called Cognigrape, which includes extracts from Vitis vinifera, in healthy adults between the ages of 55 and 75 in Italy. One group of 57 participants received 250mg of Cognigrape per day while the other group of 54 received placebo once a day for twelve weeks. Several weeks after the supplementation period, the group taking Cognigrape showed significant improvement in cognitive function compared to baseline and compared to the group taking placebo. The Cognigrape group also showed significant reductions in depression symptoms, improvements in somatic symptoms, and improvements in attention, language, immediate memory, and delayed memory. This is the first study to find an improvement in cognitive performance in humans after supplementation with a Vitis vinifera extract.
The study by Calapai and colleagues was published in the journal Frontiers in Pharmacology in 2017.
Omega-3 Fatty Acids Improve Executive Function in Youth with Mood Disorders
A 2017 study by Anthony T. Vesco and colleagues in The Journal of Child Psychology and Psychiatry suggests that in youth with depression or bipolar not otherwise specified (BP-NOS), omega-3 fatty acid supplements improve executive functioning and behavior regulation compared to placebo.
Ninety-five participants aged 7–14 years received two capsules daily of either omega-3 fatty acids (1.87g total per day, mostly consisting of EPA) or placebo for 12 weeks. Those who received omega-3s showed improvement in executive functioning (which can include planning and decision-making), behavioral regulation, and metacognition, as rated by their parents.
Editor’s Note: Since omega-3 fatty acids have no known side effects, there is little reason not to try them in youth with depression or bipolar disorder.
Omega-3 Fatty Acids Improve ADHD
 A 2017 systematic review and meta-analysis found that omega-3 fatty acid supplementation improves symptoms of attention-deficit hyperactivity disorder (ADHD) in children and adolescents. The article by Jane Pei-Chen Chang and colleagues in the journal Neuropsychopharmacology identified seven randomized controlled trials in which omega-3 fatty acids improved clinical symptoms of ADHD, and three trials in which omega-3s improved cognitive measures associated with attention.
A 2017 systematic review and meta-analysis found that omega-3 fatty acid supplementation improves symptoms of attention-deficit hyperactivity disorder (ADHD) in children and adolescents. The article by Jane Pei-Chen Chang and colleagues in the journal Neuropsychopharmacology identified seven randomized controlled trials in which omega-3 fatty acids improved clinical symptoms of ADHD, and three trials in which omega-3s improved cognitive measures associated with attention.
The meta-analysis also found that children and adolescents with ADHD have lower than normal levels of the omega-3s DHA and EPA, in addition to lower total levels of omega-3s measured in blood and cheek tissues.
Chang and colleagues suggest that omega-3 fatty acid supplementation is a potentially helpful and largely risk-free treatment option for ADHD in children and adolescents.
PTSD Increases Risk of Lupus
 A new large 2017 study in the journal Arthritis and Rheumatology reports that post-traumatic stress disorder (PTSD) in women triples their risk of developing the autoimmune disease lupus. The study included 54,763 civilian women whose health data was tracked over a period of 24 years.
A new large 2017 study in the journal Arthritis and Rheumatology reports that post-traumatic stress disorder (PTSD) in women triples their risk of developing the autoimmune disease lupus. The study included 54,763 civilian women whose health data was tracked over a period of 24 years.
Not only did PTSD increase lupus risk, but any traumatic event doubled lupus risk compared to women who were not exposed to trauma.
The researchers, led by Andrea L. Roberts, were taken by surprise at the strong links between trauma and lupus. Trauma was more of a risk factor for lupus than smoking.
Type of Trauma Affects Gene Transcription Effects in PTSD
 In a 2017 article in the journal Neuropsychopharmacology, researcher Michael S. Breen and colleagues analyzed five separate studies of post-traumatic stress disorder (PTSD) and found that sex and type of trauma affected the immunological pathways that changed with PTSD. People with PTSD showed disruptions in gene expression in specific immunological pathways depending on what type of trauma they had experienced.
In a 2017 article in the journal Neuropsychopharmacology, researcher Michael S. Breen and colleagues analyzed five separate studies of post-traumatic stress disorder (PTSD) and found that sex and type of trauma affected the immunological pathways that changed with PTSD. People with PTSD showed disruptions in gene expression in specific immunological pathways depending on what type of trauma they had experienced.
Men exposed to combat traumas showed downregulation in a pathway related to wound healing, while men who were exposed to interpersonal traumas had upregulation in a signaling pathway mediated by the inflammatory marker IL-12. Women exposed to interpersonal traumas showed upregulation of two pathways—one related to lipid metabolism and the other related to MAPK (or mitogen-activated protein kinase) activity.
The participants with PTSD also showed a lot of the same disruptions across all types of trauma, including disruptions that affected cytokine, innate immune, and type 1 interferon pathways.
These data show that immune dysregulation and inflammatory pathways play a role in the pathophysiology of PTSD.
Eye Movement Desensitization and Reprocessing Can Improve PTSD
A 2014 meta-analysis of clinical trials showed that the therapeutic technique known as eye movement desensitization and reprocessing (EMDR) can reduce symptoms of post-traumatic stress disorder (PTSD). The meta-analysis also established that longer durations of EMDR treatment correlated with better outcomes.
The meta-analysis by Ying-Ren Chen and colleagues in the journal PLOS One evaluated 26 randomized controlled trials of EMDR in people with PTSD. Chen and colleagues found that EMDR reduced PTSD symptoms, depression, anxiety, and subjective distress.
EMDR is a psychotherapeutic technique intended to reduce the distress that a patient feels about a traumatic memory. The patient is encouraged to recall the traumatic event while focusing on an external stimulus. Typically this would mean using their eyes to track the therapist’s hand moving back and forth from left to right. This process can help patients reprocess the trauma and alleviate the stress that they feel upon recalling the traumatic memory.
Chen and colleagues found that EMDR sessions that lasted longer than one hour were more effective than those that lasted less than an hour. Another finding that was that groups led by therapists who were experienced in PTSD group therapy were more effective than groups led by therapists without that experience.
Other more recent research has established that traumatic memories can be reprocessed or even extinguished by making use of the memory reconsolidation window. Five minutes to one hour after a patient engages in active emotional recall of a traumatic memory, a window of time opens in which that memory is subject to reinterpretation and revision.
An experienced therapist can create a safe environment for a patient to recall traumatic events and find alternative ways of interpreting the experience—for example, by focusing on their strength in surviving the experience. This process resembles EMDR in many ways, but without the eye movements.
In a 2017 article in the journal Psychiatry Research, BNN Editor-in-Chief Robert M. Post and colleague Robert Kegan discuss the possibility of using the reconsolidation window to reprocess stressors that led to a depressive episode.
Proton Pump Inhibitors Linked to Gastric Cancer
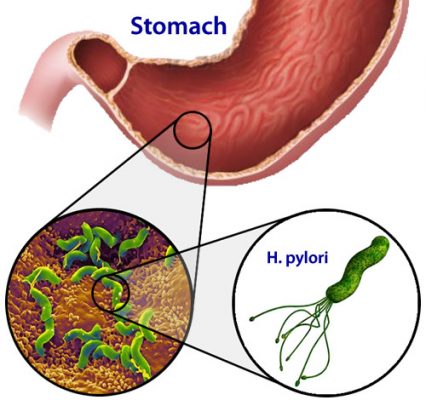 Proton pump inhibitors (PPIs), a type of medication used to reduce gastric acid, have been linked to gastric cancer in a new study by Ka Shing Cheung and colleagues. A 2017 article in Gut, the journal of the British Society of Gastroenterology, reports that receiving PPIs to treat stomach infections from the bacterium Helicobacter pylori increases the risk of later gastric cancer.
Proton pump inhibitors (PPIs), a type of medication used to reduce gastric acid, have been linked to gastric cancer in a new study by Ka Shing Cheung and colleagues. A 2017 article in Gut, the journal of the British Society of Gastroenterology, reports that receiving PPIs to treat stomach infections from the bacterium Helicobacter pylori increases the risk of later gastric cancer.
The study relied on a territory-wide health database in Hong Kong. Out of 63,397 subjects, 153 developed gastric cancer after being treated for Helicobacter pylori. PPI treatment was associated with a 2.4-fold increase in risk of gastric cancer, while treatment with histamine-2 receptor agonist drugs did not increase cancer risk.
Editor’s Note: PPIs are widely used in psychiatric patients. Care should be taken with their long-term use.
Diet Drinks May Worsen Glucose Control, Making Type 2 Diabetes More Likely
 Many people substitute diet drinks containing artificial sweeteners for sugary drinks in the hopes of reducing their diabetes risk. However, new research suggests that artificial sweeteners alter the gut’s response to glucose in a way that could actually worsen diabetes risk.
Many people substitute diet drinks containing artificial sweeteners for sugary drinks in the hopes of reducing their diabetes risk. However, new research suggests that artificial sweeteners alter the gut’s response to glucose in a way that could actually worsen diabetes risk.
At the 2017 meeting of the European Association for the Study of Diabetes, researcher Richard Young described a small study in which he and his colleagues compared the effects of artificial sweeteners to those of placebo in healthy adults. Seventeen participants consumed an amount of artificial sweetener equivalent to what would be found in 1.2 to 1.5 liters of diet beverage per day for two weeks, while 16 participants received placebo.
Young and colleagues determined that glucose absorption and glycemic response increased in the participants who consumed the artificial sweetener. Those who consumed the sweetener absorbed 20% more glucose than those in the placebo group. While before the study the two groups had similar blood glucose levels, these rose by 24% in those who consumed the artificial sweetener.
Consuming artificial sweetener also seemed to affect the gut peptide GLP-1, which limits the rise in blood glucose after meals. The two groups had similar GLP-1 responses before the study, but after consuming artificial sweetener, participants showed a 34% reduction in GLP-1 response to glucose absorbed in the intestines.
Changes like these could increase the risk of type 2 diabetes. Young explained that artificial sweeteners may reduce the body’s ability to control blood sugar levels, leading to high glucose, and possibly predisposing those who consume artificial sweeteners to type 2 diabetes. Young and colleagues have previously found that switching from sugar to artificial sweeteners does not predict a lower risk of type 2 diabetes.
This study was the first of its kind in humans. Larger studies will help to clarify the effects of artificial sweeteners on glucose control.
Adipokines May Be the Link Between Mood Disorders and Obesity
 Researchers David J. Bond and Lakshmi Yatham think they may have identified why bipolar disorder and obesity occur so often together. In North America, more than 60% of people with bipolar disorder are overweight or obese, and obesity rates are 60% higher in people with bipolar disorder than in people without bipolar disorder.
Researchers David J. Bond and Lakshmi Yatham think they may have identified why bipolar disorder and obesity occur so often together. In North America, more than 60% of people with bipolar disorder are overweight or obese, and obesity rates are 60% higher in people with bipolar disorder than in people without bipolar disorder.
Bond and Yatham hypothesized that adipokines might be responsible for both bipolar disorder and obesity. Adipokines are cell signaling proteins that regulate both mood and appetite. Abnormal levels of adipokines in blood could cause both mood episodes and weight gain.
The researchers measured blood levels of five adipokines (leptin, adiponectin, resistin, adipsin, and lipocalin-2) in 53 young people with bipolar disorder. They found three interesting links between adipokines, mood, weight, and medications, which they reported in the Journal of Clinical Psychiatry in 2017.
The first finding was that low levels of leptin and adiponectin (adipokines with antidepressant properties) predicted a greater risk of depressive relapse over a 12-month period. The second finding was that high levels of leptin and adipsin predicted greater weight gain over a 12-month period. The third finding was that treatment with second-generation antipsychotics, which often leads to weight gain and other metabolic side effects, was associated with higher levels of resistin, an adipokine linked to type 2 diabetes.
The findings about leptin were particularly interesting, because leptin’s appetite-regulating effects change with a person’s weight. In the study, low leptin predicted depression, while high leptin predicted weight gain. In people of normal weight, low leptin predicts weight gain, while in overweight or obese people, high leptin predicts weight gain. Bond and Yatham suggest that leptin’s mood-regulating effects may be more consistent, with low leptin increasing depression risk regardless of weight.
These findings may help researchers find ways of treating mood episodes that do not encourage weight gain.
Exercise in Childhood Decreases Depression Symptoms Two Years Later
A 2017 study in the journal Pediatrics found that higher rates of moderate to vigorous physical activity at ages six and eight was linked to fewer symptoms of depression at age 10.
The study included 795 six-year-olds who were tracked for four years. Their physical activity was measured by accelerometry, the same type of technology found in smartphones and other consumer products that can track a person’s daily steps. Depression symptoms were assessed via interviews with the children and their parents.
While exercise seemed to reduce depression symptoms, sedentary behavior did not predict later depression.




