Genetic Risk Factors for Onset of Bipolar Disorder
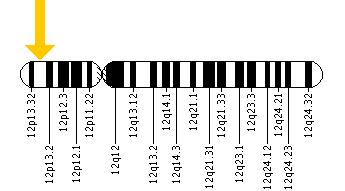
A Genetic Risk Factor For Bipolar Disorder: The CACNA1C Gene
In an abstract presented at the 5th Biennial Conference of the International Society for Bipolar Disorders, Sophia Frangou reported on the CACNA1C polymorphism, a genetic variation that has been associated with the risk of developing bipolar disorder in several genome-wide association studies that search for links between genes and illnesses. Frangou found that those people with the genetic variation had increased volume in some parts of the brain, including the right hypothalamus and the right amygdala, and decreased volume in others, including the putamen, as well as alterations in the functional connectivity of different cortical areas.
These data may be related to findings that calcium influx may play a role in bipolar disorder. In people with the genetic variation, the risk allele binds to a subunit of the voltage-dependent calcium channel, which modulates the influx of calcium from the outside to the inside the neuron.
Increased amounts of calcium are consistently found in the white cells and platelets of patients with bipolar disorder compared to controls. Moreover, the drug nimodipine, a dihydropyridine L-type calcium channel blocker, is effective in the prevention of manic and depressive episodes in a subgroup of patients, particularly those with cycling patterns that are ultra-rapid (4+ episodes per month) or ultradian (including a mood switch within a 24-hour period 4+ times per month). A large randomized study of patients with bipolar disorder presented by H.R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry also found that while lithium was associated with a 50% response rate, the combination of lithium and nimodipine was associated with a 73% response rate, again suggesting the additional efficacy of blocking L-type calcium channels.
Immune Abnormalities May Predict Onset of Bipolar Disorder in Children at High Risk
At the 5th Biennial Conference of the International Society for Bipolar Disorders E. Mesman discussed connections between immunity and bipolar disorder. Mesman and colleagues followed offspring of parents with confirmed bipolar disorder for 12 years and compared them to children in the general population. In the children of bipolar parents they found higher levels of immune markers called cytokines (PTX3 and sCD25) in circulating monocytes, a type of white blood cell. In the children of bipolar parents they also found a high inflammatory setpoint in the monocytes. T-effector and T-regulatory cells were also different in the offspring of bipolar parents.
While these findings were present in children who had already become ill with bipolar disorder, they were also present in those who had yet to experience a mood disorder, suggesting that these immune and inflammatory markers may ultimately be an important risk marker for the onset of bipolar disorder.
Editor’s Note: These are among the first studies suggesting that immune and inflammatory abnormalities may precede the onset of bipolar disorder. Many studies have shown that patients with active bipolar disorder show more inflammation, including increases in inflammatory markers interleukin 1 (IL-1), interleukin 6 (IL-6), C reactive protein (CRP), and tumor necrosis factor alpha (TNFa). The new data are of considerable importance not only because inflammation could serve as a marker of illness onset, but also because inflammation could become a potential target for therapeutics (i.e. using anti-inflammatory and immune-suppressing agents to treat bipolar disorder).
Genetic Markers of Response to Lithium
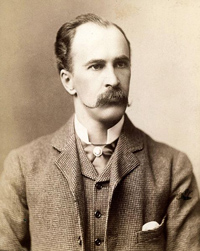
 At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
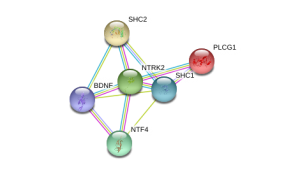
In his research Kelsoe found that a variant of the gene that codes for neurotrophic receptor type II (NTRK2), the receptor for brain-derived neurotrophic factor (BDNF), was associated with good response to lithium in patients with a family history of bipolar disorder or a history of euphoric mania. The “T” allele of rs1387923 was associated with better response to lithium retrospectively, and these results were replicated in a prospective study.
Editors Note: These data are among the first to indicate that genetic information could be used to make treatment decisions. Lithium increases BDNF and neurogenesis, thus it makes some sense that a variation in the BDNF receptor would affect clinical responsiveness to lithium.
In a similar vein, Janusz K. Rybakowski reported at the Society of Biological Psychiatry meeting on another possible predictor of long-term excellent response to lithium in bipolar disorder. Due to normal genetic variation, different people have different versions of BDNF. Rybakowski found that the patients with a version of BDNF known as Val66Val who had bipolar disorder performed significantly better on the Wisconsin Card Sorting Test, which evaluates abstract reasoning. However, he found that patients with a methionine amino acid in the place of one of the valine amino acids (resulting in a Val66Met allele, which is associated with minor cognitive difficulties) showed significantly better response to preventative treatment with lithium. It is noteworthy that these excellent lithium responders also performed better on a complex neuropsychological battery than those who were less good responders to lithium. The good responders’ performance on these tests was not different from healthy controls.
Editor’s Note: These data add to the possibility that prediction of lithium response is linked to common gene variations in neuroprotective factors or their receptors. It is interesting that the patients with the Val66Met allele, which works less efficiently, show the best long-term response to lithium. This is consistent with the view that lithium, which increases BDNF, is most effective in those who have a sluggish functioning of their BDNF due to having the Met allele. As we have written before, those with the Met allele have slight decrements in working memory, and in animal models, those with the Met allele show deficits in long-term potentiation (LTP), which suggest problems with long-term memory. Thus, using lithium to increase BDNF function in those with a “sluggish” variation in their BDNF makes sense and may ultimately be clinically useful.
Switch your print subscription to digital today!
 Help us save printing and mailing costs and paper by switching your print subscription to an email subscription today. Email info (at) bipolarnews (dot) org with your zip code and your email address!
Help us save printing and mailing costs and paper by switching your print subscription to an email subscription today. Email info (at) bipolarnews (dot) org with your zip code and your email address!
You’ll still receive the same content in our quarterly newsletter, only now in your email inbox. Or stay up to date on the latest developments in the treatment of mood disorders via this blog or by following our Twitter account.
The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more
Comments on Treatment Conundrums
Clinical medicine is an art and as medical pioneer Sir William Osler declared, often involves “skillful use of combinations.” As the risks of inadequately treated illness increase, use of drugs with inadequately delineated benefit-to-risk ratios may be increasingly justified, such as in the case of memantine as recommended by Koukopoulos.
One should start early, effective, preventive pharmacological treatment of the recurrent unipolar and bipolar disorders. When this is not accomplished, an increasing number of unknowns enter the treatment equation, and as these illnesses enter more serious stages of recurrence, progression, and treatment resistance, the path to remission and wellness becomes increasingly complicated and relies on skillful management, guesswork, and good data from patients.
Given the multiple unknowns, patients can play an important role. They can be intimately involved in the decision-making, and provide precise feedback in the formal or informal longitudinal monitoring of mood, sleep, other symptoms, and side effects so that whatever is tried can be accurately assessed. A treatment with known efficacy is only worthwhile if it is effective in a given patient. When evidence of efficacy in the literature is more questionable, the evidence of effectiveness of a given treatment regimen in a given individual becomes all the more important to discern. We recommend that patients chart their mood and medications using the National Institute of Mental Health’s Life Charting Method (NIMH-LCM) or another type of personal calendar (we offer several on our Lifecharting page–see the gray horizontal menu above this article). This type of careful longitudinal monitoring method can help in the quest for an optimal treatment result.
Our old recommendation would appear particularly appropriate for this discussion. When things are going well (in the treatment of recurrent mood disorders), be conservative and stay the course. Conversely, when mood is not stabilized, be more radical and continue to explore new options until stability is achieved.
When Added to Valproate, Memantine Increased HDLs (“Good” Cholesterol) But Did Not Enhance Effectiveness of Treatment
R.B. Lu and S.Y. Lee reported in a poster at the 5th Biennial Conference of the International Society for Bipolar Disorders in 2012 that adding memantine (Namenda) to treatment with valproate (Depakote) was associated with increases in high-density lipoproteins (HDLs) or “good” cholesterol in bipolar II depressed patients. However, the combination was no more clinically effective than valproate alone in treating the patients’ bipolar illness, as had been hoped.
Editor’s Note: These data on memantine’s failure to improve patients’ bipolar illness when used as an adjunct to valproate contrast with those of Amit Anand et al., who reported in 2012 that memantine was a partially successful adjunctive treatment when added to ongoing treatment with lamotrigine. This combination of lamotrigine plus memantine was associated with faster and more robust antidepressant effects than the combination of lamotrigine plus placebo in patients with bipolar depression. This effect was significant in the first four weeks of the study as the dose of memantine was slowly increased from 5mg/day to 20mg/day, but not over the last four weeks of treatment at 20 mg/day.
The data of Anand et al. makes theoretical sense. Since lamotrigine inhibits the release of glutamate and memantine inhibits the actions of glutamate at the NMDA receptor, the two together might produce additive decrements in glutamatergic actions through two different mechanisms. In contrast, valproate is more closely associated with increases in GABAergic mechanisms, and this may explain why its effects on bipolar disorder were not improved by the addition of memantine.
Print Archives are Available!
It was brought to our attention that there was a problem with the most recent link in our print archives, and now it is fixed. You can download Volume 16, Issue 3 here, along with any past issue dating back to 1995. (If you are an email subscriber you have already received this issue’s content, and if you are a print subscriber you should be receiving this issue in the mail any day now!)
Anti-Alzheimer’s Drug Memantine (Namenda) Has Positive Effects On Cognitive Dysfunction In Patients With Bipolar Disorder
 Many patients with bipolar disorder experience cognitive dysfunction, but few treatments are available for this aspect of the illness. In an abstract presented at the 67th Annual Meeting of the Society of Biological Psychiatry in 2012, Dan V. Iosifescu reported that in a randomized 12-week study in which the anti-Alzheimer’s drug memantine was given to 72 euthymic bipolar subjects experiencing cognitive deficits, the drug was associated with improvement in spatial and working memory, verbal and episodic memory, and other indices that included measurements of attention and language skills. In conjunction with this treatment, a subgroup of subjects had increases in left hippocampal NAA (a measure of neuronal viability) and increases in choline in the right hippocampus. The initial improvements in these neuropsychological test results remained over 12 weeks of open follow-up.
Many patients with bipolar disorder experience cognitive dysfunction, but few treatments are available for this aspect of the illness. In an abstract presented at the 67th Annual Meeting of the Society of Biological Psychiatry in 2012, Dan V. Iosifescu reported that in a randomized 12-week study in which the anti-Alzheimer’s drug memantine was given to 72 euthymic bipolar subjects experiencing cognitive deficits, the drug was associated with improvement in spatial and working memory, verbal and episodic memory, and other indices that included measurements of attention and language skills. In conjunction with this treatment, a subgroup of subjects had increases in left hippocampal NAA (a measure of neuronal viability) and increases in choline in the right hippocampus. The initial improvements in these neuropsychological test results remained over 12 weeks of open follow-up.
Editor’s Note: These data are of considerable importance. Many studies indicate that the severity of the cognitive dysfunction patients experience while euthymic varies directly as a function of the number of prior episodes of mania or depression they have experienced. The degree of cognitive dysfunction in patients with bipolar disorder is also correlated with disability in social and economic functioning. Thus, the data that memantine can lead to improvement in several types of memory tests suggest that the drug could be useful in treating these deficits in some patients with bipolar disorder.
Memantine acts in part by blocking glutamate NMDA receptors and provides a different mechanism of action compared to the other drugs used to treat Alzheimer’s, which increase acetylcholine by blocking acetylcholinesterase.
Memantine has also shown promising effects in enhancing the antidepressant effects of lamotrigine, a drug that inhibits glutamate release. Thus, the similar target of action by which lamotrigine (blocking glutatmate release) and memantine (blocking glutamate receptors) operate suggest that the two drugs used in conjunction might produce additive effects in decreasing glutamate function. The current data suggest that memantine compared to placebo as an add-on to other agents in euthymic bipolar patients improves several measures of cognition as well.
New data published by Koukopoulos in the Journal of Affective Disorders in 2012 suggest that memantine (10-30mg/day) is an effective add-on treatment in severely ill patients with treatment-resistant bipolar disorder. Among those in Koukopoulos’ study, 72.5% were much or very much improved, thus there is a strong rationale for considering this drug.