Genetic Markers of Response to Lithium
 At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
At the 5th Biennial Conference of the International Society for Bipolar Disorders and the 67th Annual Meeting of the Society of Biological Psychiatry, John Kelsoe presented his research on personalized pharmacotherapy for bipolar disorder, describing genetic predictors of response to lithium.
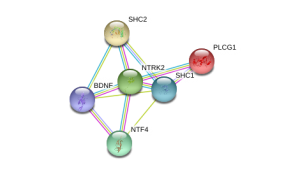
In his research Kelsoe found that a variant of the gene that codes for neurotrophic receptor type II (NTRK2), the receptor for brain-derived neurotrophic factor (BDNF), was associated with good response to lithium in patients with a family history of bipolar disorder or a history of euphoric mania. The “T” allele of rs1387923 was associated with better response to lithium retrospectively, and these results were replicated in a prospective study.
Editors Note: These data are among the first to indicate that genetic information could be used to make treatment decisions. Lithium increases BDNF and neurogenesis, thus it makes some sense that a variation in the BDNF receptor would affect clinical responsiveness to lithium.
In a similar vein, Janusz K. Rybakowski reported at the Society of Biological Psychiatry meeting on another possible predictor of long-term excellent response to lithium in bipolar disorder. Due to normal genetic variation, different people have different versions of BDNF. Rybakowski found that the patients with a version of BDNF known as Val66Val who had bipolar disorder performed significantly better on the Wisconsin Card Sorting Test, which evaluates abstract reasoning. However, he found that patients with a methionine amino acid in the place of one of the valine amino acids (resulting in a Val66Met allele, which is associated with minor cognitive difficulties) showed significantly better response to preventative treatment with lithium. It is noteworthy that these excellent lithium responders also performed better on a complex neuropsychological battery than those who were less good responders to lithium. The good responders’ performance on these tests was not different from healthy controls.
Editor’s Note: These data add to the possibility that prediction of lithium response is linked to common gene variations in neuroprotective factors or their receptors. It is interesting that the patients with the Val66Met allele, which works less efficiently, show the best long-term response to lithium. This is consistent with the view that lithium, which increases BDNF, is most effective in those who have a sluggish functioning of their BDNF due to having the Met allele. As we have written before, those with the Met allele have slight decrements in working memory, and in animal models, those with the Met allele show deficits in long-term potentiation (LTP), which suggest problems with long-term memory. Thus, using lithium to increase BDNF function in those with a “sluggish” variation in their BDNF makes sense and may ultimately be clinically useful.
The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more


