Paternal heroin self-administration in rats increases drug-seeking behavior in male offspring via miR-19b downregulation in the nucleus accumbens
Wenjing Gao et al reported in Neuropsychopharmacology (2025) that “paternal heroin self-administration in rats results in increased heroin-seeking behavior in F1 male offspring. This effect was replicated by zygotic microinjection of sperm RNAs from heroin self-administration-experienced rats, but not from yoked infusion pairs, highlighting the role of sperm non-coding RNAs changes induced by paternal drug-seeking behavior (and not by just passive receipt of heroin.) Analysis of non-coding RNA changes in the NAc [nucleus accumbens] and sperm of the F0 generation revealed a significant correlation in miRNA expression profiles, particularly the downregulation of miR-19b in both tissues, which was linked to the observed phenotype. The heightened heroin-seeking behavior in the male F1 generation could be reversed by supplementing synthetic miR-19b in F0 sperm RNA or introducing miR-19b into the NAc of F1 offspring. These findings suggest that sperm miRNAs like miR-19b mirror changes in brain miRNAs, participate in epigenetic transmission of acquired traits from F0 to F1, as well as in regulating heroin SA behavior of offspring.”
Editor’s Note: These data suggest that dad rats self administering heroin transmit a vulnerability to self administering heroin to their offspring. It does not occur if the dad rats merely get heroin passively. It is likely that these data could be extrapolated to humans. If so, there is a question of whether taking opiates for pain (administered by a nurse as opposed to self administrated) would transmit vulnerability to the offspring. In any event, it may be that a heroin addict who self administers the drug not only puts himself at risk but also his male offspring. This makes clear that methods of producing primary protection in offspring for opiate addiction deserve exploration
Review: Reconsideration of bipolar disorder as a developmental disorder
Reconsideration of bipolar disorder as a developmental disorder: Importance of the time of onset
Pierre Alexis Geoffroy et al, J Physiology Paris, 2013
Eight admixture studies have demonstrated three homogeneous subgroups of patients with bipolar disorder, identi?ed by their age at onset (early, intermediate and late age at onset), with two cutoff points, at 21 and 34 years.
The early onset group had more: Suicide attempts, rapid cycling, drug and alcohol abuse, psychotic symptoms, panic disorder, OCD, and a positive family history for affective disorder. Early onset illness should be recognized and treated earlier.
THE PATHOPHYSIOLOGY OF SCHIZOPHRENIA IS BECOMING CLEARER
David Lewis of U. Pittsburgh showed that the glutamate neurons in the prefrontal cortex of patients with schizophrenia are deficient in the gamma (30-50 Hz) oscillations that are responsible for normal working memory.
Not only are dendrites and spines deficient in these neurons in layer 3 of the cortex, but there is a deficit in parvalbumin GABA inhibitory neurons. The GABA enzyme GAD 67 is lower, producing less inhibition. The frontal neurons are hypoactive and there is less BDNF and oxidative phosphorylation present, yielding decreases in mitochondrial function.
Influence of Childhood Maltreatment on Morphometry and Brain Network Architecture in Bipolar Disorder
Martin Teicher of McLean Hospital, Harvard Medical School, reported on the influence of childhood maltreatment on morphometry and brain network architecture in Bipolar Disorder.
“Childhood maltreatment (MAL) is common in individuals with bipolar disorder (BP) and is associated with earlier onset, more severe course, and more comorbidities.” They found that reduced hippocampal volume and white matter alterations were present in those with a history of childhood maltreatment. They concluded that “MAL may act as a sensitizer promoting the emergence of bipolar symptoms in individuals with less severe network abnormalities” than in BP patients with no MAL.
Lithium Is Unparalleled in It Range of Efficacy in the Mood Disorders
Most clinicians are aware of lithium’s superiority over other mood stabilizers in bipolar illness prophylaxis. New data suggests this might also apply to the atypical antipsychotics.
Lithium is also not only an effective adjunct to antidepressant in unipolar depression, but has some of the best data for its use in long term prevention. In bipolar disorder prophylaxis it is particularly effective in those with classical presentations of discrete episodes of euphoric mania, treatment early in the course of illness, lack of anxiety and substance comorbidities, and a positive history of mood disorder in first-degree relatives.
New data indicates that it is also effective in childhood onset mania, and open long term follow ups indicate that it is more effective than other mood stabilizers or atypical antipsychotics.
Despite the compelling effectiveness data and many ancillary benefits, survey data indicates very low levels of current lithium use in both adult and child bipolar disorder. The conventional view, shared by most patients and many clinicians, underestimates its range of effectiveness and potential benefits while overestimating it is side effects. A more balanced view is needed as neglect of wider use of lithium is detrimental to the long term outcome of immense numbers of patients.
Robert M. Post, MD
“Epigenetic Changes After Trauma May Be Adaptive, Contribute to Resilience”
Originally From Psychiatric News Update
In recent years, research throughout the scientific and medical community has suggested a link between trauma and epigenetic changes, chemical modifications that affect gene activity without actually changing the gene’s DNA sequence. The assumption has been that epigenetic changes in the context of trauma are inherently bad, a form of damage that gets passed from generation to generation. But according to Rachel Yehuda, Ph.D., Endowed Professor of Psychiatry and Neuroscience of Trauma at the Icahn School of Medicine at Mount Sinai, these changes may also be adaptations that promote resilience.
“Sometimes the biological changes in response to trauma or intergenerational trauma are there to help deal with the problem of trauma, not compound its effects,” Yehuda said. “The survival advantage of this form of intergenerational transmission depends in large part on the environment encountered by the offspring themselves.”
Yehuda described this phenomenon as a paradox.
“Parental or ancestral trauma may heighten vulnerability to mental health challenges, but epigenetic adaptations may simultaneously facilitate coping mechanisms,” she said. “Trauma increases susceptibility for psychological distress, but also produces adaptations that help us cope with them.”
Yehuda described research she and her colleagues have conducted to tease out how trauma in parents can affect offspring in the context of the biology of posttraumatic stress disorder (PTSD) in Holocaust survivors and their children. As the research unfolded, Yehuda and colleagues found that survivors’ adult children were more likely to have mood disorders, anxiety disorders, and PTSD than Jewish people whose parents did not directly experience the Holocaust. This was especially true of children of Holocaust survivors who had PTSD. The researchers also found that many children of Holocaust survivors had low levels of the stress hormone cortisol, particularly if their parents had PTSD.
Yehuda and colleagues then conducted a series of studies that looked at the role of glucocorticoid receptors — the proteins to which cortisol must bind to exert its effects — and found evidence that these receptors were more sensitive in people with PTSD.
“In practical terms this means that even though someone with PTSD might have lower circulating levels of cortisol in their blood, their cells might react more strongly to the cortisol that is present,” Yehuda said.
Yehuda said that epigenetics provided further insight on the relationship between hypersensitive glucocorticoid receptors, cortisol, and PTSD. She explained the potential role of methylation, which is a chemical reaction in the body in which a small molecule called a methyl group gets added to DNA or DNA-associated proteins.
“Increased methylation generally impedes RNA transcription, whereas less methylation enhances gene expression,” Yehuda said.
In 2015, Yehuda and colleagues conducted a study involving combat veterans who had PTSD and found lower methylation on an important region on the participants’ glucocorticoid receptor gene. The changes were associated with cortisol and glucocorticoid receptor sensitivity in the study participants, suggesting a potential epigenetic explanation for the association between the trauma of combat and PTSD.
Yehuda said that stress-related epigenetic changes may be reversible. For example, one of the studies conducted by her team revealed that combat veterans with PTSD who benefited from cognitive-behavioral psychotherapy showed treatment-induced changes in the methylation of a gene that regulates glucocorticoid receptor sensitivity. Yehuda said that this finding confirmed that healing is also reflected in epigenetic change.
“That we can transform to meet environmental challenge is a superpower. That is resilience,” Yehuda said.” ?
Yehuda then went on to describe the striking and lasting effects of the psychedelics psilocybin and MDMA in trauma and in helping patients confront their fears in a positive and hopeful fashion. These agents which are given with intensive psychotherapeutic support are not yet FDA approved, but preliminary data suggest that they can have dramatic therapeutic effects in trauma and depression. They can help patients change their attitudes to themselves and the world.
LITHIUM IS VASTLY UNDER-UTILIZED IN BIPOLAR DISORDER LEADING TO PREMATURE DEATH AND DISABILITY: WE WANT YOU TO HELP REVERSE THIS ANOMALOUS TREND
We are looking for people who have had a good course of illness with lithium included in their treatment regimen to help spread the word that lithium works extremely well and its side effects are erroneously overestimated.
We are hoping that you, as a good responder to lithium, will start a positive chain letter to fellow patients, family members, and friends suggesting that earlier and greater use of lithium would be overwhelmingly likely to improve the lives of many individuals with bipolar illness.
Why do we need you? It is because every expert in the treatment of bipolar illness of whom I am aware of has long advocated for greater and earlier use of lithium, but with little success. Lithium is widely recognized as a first line and treatment of choice for bipolar disorder, yet its use remains miniscule. In the US somewhere between only 10 to 27% of bipolar patients are given lithium. This has tragic consequences.
Treatment outcomes of the illness remain poor with vast numbers of patients experiencing pain, disability, memory loss, and loss of many years of life expectancy from suicide, cardiovascular disease, and many other psychiatric and medical disabilities. Compared to the general population, people with bipolar illness lose between 10-15 years of life expectancy. A new study by Carvalho et al (Psychother Psychosom, 2024) of more than 50,000 patients with a first episode of mania compared to more than 250,000 matched controls have a significantly higher rate of all cause mortality and a 10 fold increase of suicide. Those treated with lithium have a significantly lower rate of both all cause mortality and of suicide.
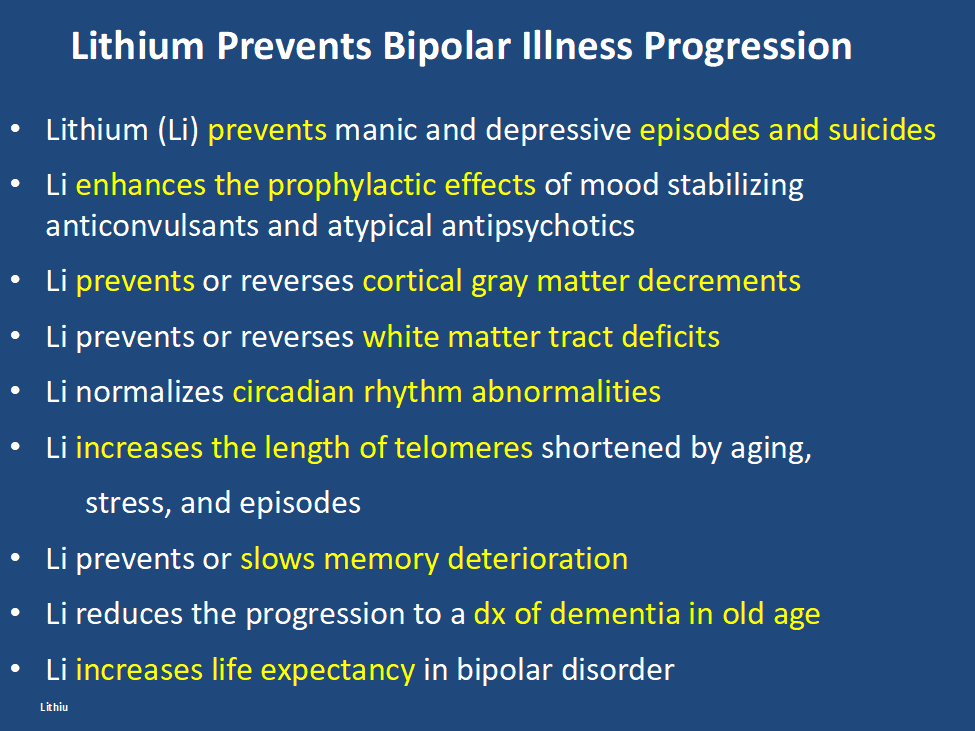
In addition, lithium has many other assets, besides the treatment of mania, of which most people are unaware and the liabilities of its side effects profile are over estimated. Some of the positive’s of lithium are listed below. Please print this ‘list of assets of lithium out and give it to everyone who might be interested. Patients with bipolar disorder should also print it out for their treating physicians, particularly if they do not as yet have lithium in their treatment regimen.
At the same time lithium’s side effects are over emphasized. The biggest concern is that lithium causes end stage kidney dysfunction eventually leading to dialysis. This is likely based on findings that individuals with bipolar disorder have an increase in most medical illnesses including chronic kidney disease compared to the general population. However, two very large trans-national studies of bipolar patients in Denmark and in Israel have found that bipolar patients treated with lithium are no more likely to get end stage renal disease than those treated with anticonvulsants such as valproate (Depakote). Lithium does cause low thyroid function in 15-25% of patients, but this is easily corrected with replacement of thyroid hormone. Many other side effects of lithium such as tremor can be managed by using lower doses.
Bottom line: Lithium gets a bad rap.
Please tell everyone you know about the new data on lithium’s relative safety and its many assets including reducing all cause mortality and suicide and restoring many years of lost life expectancy. 14 of 15 studies indicate that if lithium is started early in course of bipolar disorder it is more effective than starting it after many episodes or rapid cycling have occurred. It also works well in youngsters with bipolar disorder and better in comparison to other treatments (Hafeman et al 2020). In addition, after a first mania, patients randomized to a year of treatment with lithium do better on all outcome measures than those given a year on quetiapine (Seroquel) including manic and depressive severity, functioning, cognition, and normality of brain imaging (Berk et al 2017).
One more conceptual breakthrough: Lithium is literally the original salt of the earth. It was generated just 20 minutes after the big bang origin of the universe and is considered an essential element. Common table salt, sodium chloride, emerged only many millions of years after the big bang. Also in six studies across multiple countries, higher minute levels of lithium in the drinking water have been shown to reduce the incidence of suicide in the general population. A very low dose of lithium 150-300mg/day has also been shown to reduce the progression of mild cognitive impairment in otherwise well elderly volunteers.
Do a good thing for other people. Relay this new view of lithium to everyone you can think of in hope that they will help get the word out to many others and improve the life, functioning, and longevity of those with bipolar disorder.
Suggest and promulgate a new mantra:
“LITHIUM PREVENTS EPISODES OF BIPOLAR ILLNESS, AND PROTECTS THE BRAIN AND BODY”
Bipolar I patient show dramatic reductions in white matter integrity
Thiel et al in Neuropsychopharmacology (2024) reported that “Compared with HC [healthy controls], BD-I patients exhibited lower FA [fractional anisotropy] in widespread clusters (ptfce-FWE?< 0.001), including almost all major projection, association, and commissural fiber tracts. BD-II patients also demonstrated lower FA compared with HC, although less pronounced (ptfce-FWE?=?0.049).”
Editors Note: These data once more emphasize the importance of using lithium (Li) in bipolar disorder as it can ameliorate the deficits in white matter integrity that are so prominent in the illness. Li also improve the loss of cortical grey matter volume that evolves with illness progression. Li prevents episodes of depression and mania and reduces the incidence of suicides. That Li can reverse or ameliorate brain abnormalities in bipolar disorder is one more piece of evidence that Li should be considered a disease modifying drug (DMD) and started early in the course of illness in almost all bipolar patients. The new mantra for patients and clinicians is: Use more lithium and prevent illness progression.
Cannabis Contributes to 15% of Case of Schizophrenia
A study in Psychological Medicine (May 2, 2023) reported on ” Danish registry data spanning five decades and representing more than 6.9 million people in Denmark to estimate the population-level percentage of schizophrenia cases attributable to (cannabis use disorder) CUD. A total of 60,563 participants were diagnosed with CUD. Three quarters of cases were in men; there were 45,327 incident cases of schizophrenia during the study period. The researchers estimate that in 2021, about 15% of schizophrenia cases among males aged 16 to 49 could have been avoided by preventing CUD, compared with 4% among females in this age range. For young men aged 21 to 30, the proportion of preventable schizophrenia cases related to CUD may be as high as 30%, the authors report.”
Editors Note: Other data also support an increased risk for bipolar disorder in those abusing cannabis. The notion that cannabis use carries few risks is baloney. Making pot legal does not make it safe.
Assets of Exercise
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Ben Goldstein of the University of Toronto gave a plenary talk on the benefits of exercise.
He found poor aerobic fitness in 19 of 20 young bipolar patients. They had low cerebral blood flow in proportion to the severity of their exhaustion after exercise. He noted the importance of stressing an endpoint of fitness for exercise rather than weight loss. Using an exercise coach and running with family and friends was helpful in motivating patients for consistent exercise.

