Recovery and Relapse After a First Mania
The timeframe during which recovery and recurrence occur in people with a first episode of mania are somewhat variable. A meta-analysis by Andréanne Gignac and colleagues published in the Journal of Clinical Psychiatry in 2015 offers some new information. The meta-analysis included eight studies with a total of 734 participants in a first episode of mania. Syndromal recovery rates (when patients no longer met diagnostic criteria for bipolar disorder) were 77.4% at six months after first episode of mania and 84.2% at one year after. However, some symptoms lingered, and only 62.1% of patients reached a period of symptomatic recovery within one year.
Recurrence rates were 25.7% within six months, 41.0% within one year, and 59.7% by four years. Those who were younger at the time of the first episode were at higher risk for relapse within one year.
Editor’s Note: On the positive side, most recovered, but on the negative side, at one year, 60% remained symptomatic and 40% had a recurrence. What is not clear is how intensively patients were treated and monitored. The main message of this study is that a first episode of mania is not trivial and deservces concerted acute and long-term treatment. When expert multimodal treatment is given results are vastly more superior than treatment as usual (Kessing et al. British Journal of Psychiatry 2013).
Collaborative Care and Education Reduces Bipolar Depression
There is increasing evidence that patients with bipolar disorder benefit from special programs or clinics designed to teach them skills to cope with their illness. A 2015 article by Trijntje Y.G. van der Voort and colleagues in the British Journal of Psychiatry evaluated the effectiveness of a Dutch program that provided collaborative care to people with bipolar disorder.
One hundred thirty-eight patients in an outpatient clinic were randomized to receive either treatment as usual or a program of nurse-provided collaborative care that included psychoeducation, problem-solving treatment, systematic relapse prevention contracts, and monitoring of outcomes. These services were managed by mental health nurses. Those patients who received collaborative care had significantly less time with depressive symptoms at the 6-month and 12-month marks, and less severe depressive symptoms at 12 months (all findings with p values less than .01).
There was no significant difference in manic symptoms or treatment adherence. The authors suggest that collaborative care improves treatment for people with bipolar disorder, especially depression, which is most closely linked to impaired quality of life and disability.
Editor’s Note: Given this study and about a dozen others like it, it is time to conclude that psychoeducation and other components of collaborative care noted here are critical to the long-term management of bipolar disorder. Patients and their family members should insist that this be a part of routine care.
Specialty Treatment for First Episodes of Psychosis Effective
A study published online in the journal Psychiatric Services comparing a specialty clinic that provides medication, family education, cognitive-behavioral therapy (CBT), and case management to improve employment and educational outcomes with treatment as usual for people in a first episode of psychosis found that the specialty treatment was associated with fewer and shorter hospital stays and better vocational engagement during one year of follow-up.
Most participants were referred to the study from inpatient psychiatric units. Those randomly assigned to receive treatment as usual typically did so in outpatient treatment settings. Those randomly assigned to the specialty treatment group joined the Specialized Treatment Early in Psychosis (STEP) program at the Connecticut Mental Health Center, where they could choose from any of the available interventions.
Other studies have found that comprehensive intervention encompassing psychoeducation, family therapy and other services can reduce psychotic symptoms. The authors of this study, Vinod H. Srihari and colleagues, concluded that a US public-sector model of early intervention in psychotic illness could be both feasible and effective.
Editor’s Note: In the British Journal of Psychiatry in 2013, Kessing et al. demonstrated even more dramatic and persistent benefits (for at least 6 years) of 2 years of specialty clinic care versus treatment as usual for patients with a first hospitalization for mania (many of whom were also psychotic). Together these two articles indicate the extreme importance of getting off to a good start in the management of major psychiatric illness. Such specialty programs are desperately needed for better management of childhood-onset mania.
Meta-Analysis Shows Effectiveness of Ketamine for Bipolar and Unipolar Depression
Ketamine, an anesthetic sometimes used intravenously in the treatment of depression, can bring about rapid onset of antidepressant effects. A new meta-analysis by researcher Michael Bloch and colleagues presented at a recent conference showed that ketamine’s maximum antidepressant effects occur within one day of administration, and its effects remain significant (compared to control conditions) one week following infusion. Ketamine’s effects were diminished in patients taking other medications. There was a trend for better response in patients with bipolar disorder than with unipolar disorder.
Bloch and colleagues analyzed eight earlier studies including a total of 180 participants. In each study, ketamine had been compared to a control condition, either an infusion of saline solution or of midazolam, which mimics ketamine’s sensory effects but does not have antidepressant effects. The researchers are calling for more meta-analyses of ketamine studies to determine which patients respond best to ketamine and how to sustain ketamine’s effects.
Editor’s Note: In another poster presented at the same conference, James Murrough reported that patients with slower processing speed responded best to ketamine. Other findings have shown that those with a history of alcohol abuse and a common genetic variant of brain-derived neurotrophic factor (BDNF), the val-66-val allele of proBDNF, are more likely to respond to ketamine.
High Blood Pressure is a Marker of Good Response to Prazosin in PTSD
Prazosin, an alpha-1 adrenoreceptor antagonist, has been found to be effective at reducing symptoms of post-traumatic stress disorder (PTSD), including nightmares. Researchers led by Murray Raskind hypothesized that there may be a link between blood pressure and response to prazosin, since resting blood pressure can be used to measure alpha-1 adrenoreceptor responsiveness. In a study of active duty combat soldiers with PTSD, higher resting blood pressure and smaller drop in blood pressure when going from lying down to standing up predicted a better response to prazosin.
The researchers believe that blood pressure can be used to estimate the central nervous systems’s responsiveness to norepinephrine, which prazosin blocks. In patients with PTSD who received placebo instead of prazosin, blood pressure did not predict improvement. Raskind and colleagues hope to be better able to predict response to prazosin in PTSD by measuring patients’ baseline blood pressure.
Ziprasidone Added to Escitalopram Improved Unipolar Depression
In a new study of patients with major depressive disorder who did not improve after eight weeks of the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram, the addition of the atypical antipsychotic ziprasidone improved their depression more than did placebo. Patients took the combination of escitalopram (20mg/day on average) and ziprasidone twice a day at doses of 20–80 mg.
This was the first randomized, double-blind placebo controlled trial of ziprasidone as an adjunct treatment for unipolar depression. While ziprasidone was more efficacious than placebo, discontinuation of the study due to intolerance was higher among the patients who received ziprasidone.
Editor’s Note: Two atypical antipsychotics (quetiapine and aripiprazole) have been approved by the Federal Drug Administration for augmentation of antidepressants in unipolar depression. Now there have also been placebo-controlled positive trials of two others (ziprasidone and cariprazine).
These findings are of particular interest as the studies of ziprasidone monotherapy in bipolar depression not only failed, but response to ziprasidone and placebo was virtually identical (and negligible).
More Evidence for Cariprazine’s Efficacy in Bipolar Depression
In an eight-week study of the drug cariprazine for bipolar depression by Joe Calabrese and colleagues, patients who received 1.5mg/day doses of the drug showed more improvement in their illness and higher remission rates after six weeks than patients who received placebo. Side effects were rare, with mild or moderate akithisia (restless legs) being most common. Cariprazine is a dopamine D3 and D2 receptor partial agonist with preferential binding to D3 receptors.
Transcranial Direct Current Stimulation May Improve Cognition in Schizophrenia
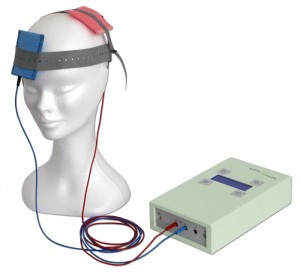 A recent study by Robert Smith and colleagues studied the use of transcranial direct current stimulation (tDCS) in patients with schizophrenia. TDCS is very low level current that has a positive (anode) or negative (cathode) electrode. Anodal stimulation of the cortex is usually associated with positive effects on mood and cognition. Patients received either five sessions of active tDCS for 20 minutes (at 2 milli Amps) or a sham stimulation for the same period. Then, one day after the final session, the patients were measured on a variety of scales for cognition and illness. Patients who received the active tDCS showed more improvements in working memory and attention than patients who received the sham treatment.
A recent study by Robert Smith and colleagues studied the use of transcranial direct current stimulation (tDCS) in patients with schizophrenia. TDCS is very low level current that has a positive (anode) or negative (cathode) electrode. Anodal stimulation of the cortex is usually associated with positive effects on mood and cognition. Patients received either five sessions of active tDCS for 20 minutes (at 2 milli Amps) or a sham stimulation for the same period. Then, one day after the final session, the patients were measured on a variety of scales for cognition and illness. Patients who received the active tDCS showed more improvements in working memory and attention than patients who received the sham treatment.
There was no difference in the two groups’ schizophrenic symptoms, including hallucinations. Smith and colleagues suggest that the improvements in cognition may result from changes to brain connectivity networks, since abnormalities in these networks have been identified in patients with schizophrenia and bipolar disorder.
Replications of this type of study are needed to clarify the effect of tDCS on cognition in schizophrenia, but given the safety and convenience of the procedure, the findings are promising.
Exercise Improves Fitness, May Help Reduce Cocaine Use
In studies of rodents, running on a wheel reduces cocaine self-administration. A recent study by Richard de la Garza and colleagues investigated whether running or walking on a treadmill can reduce cocaine cravings and use in humans. In the study of 24 participants who had been using cocaine an average of 19.7 years, participants were randomized to run, walk, or sit for 30 minutes three times per week for four consecutive weeks. After exercising, the participants reported having less craving for cocaine. Fitness measures such as body weight and resting heart rate improved in both walkers and runners. While not statistically significant, by the end of the study there was a trend indicating that exercise improved abstinence from cocaine and decreased daily craving for cocaine.
Editor’s Note: Exercise Increases brain-derived neurotrophic factor (BDNF) and neurogenesis. In rodents, cocaine is associated with decreases in BDNF in the frontal cortex, and injecting BDNF there decreases cocaine seeking. Whether this BDNF effect or the general effects of exercise on mood and conditioning account for these positive cocaine effects remains to be ascertained.
Exposure to Stress Hormone Leads to Poor Decision-Making
Adolescence may be a period of particular vulnerability to the effects of stress. New research by Shannon Gourley indicates a possible mechanism for this vulnerability. When Gourley exposed adolescent mice to low levels of the stress hormone corticosterone (the equivalent to human cortisol), they developed habit-based rather than goal-oriented decision-making, leading to behaviors that resembled human depression, which lasted into adulthood. Adult mice that were exposed to the low levels of corticosterone were not affected by it.
Gourley also used an alternative method of producing these stress responses a second time by silencing the trkB receptor for brain-derived neurotrophic factor (BDNF) in the amygdala and hippocampus of the mice. The depression-like behaviors that resulted, such as lack of motivation, were able to be reversed by treating the mice with 7,8-dihydroxyflavone, a drug that activated the trkB receptor. In the adolescent mice, this treatment had antidepressant effects that lasted into adulthood, even though the treatment stopped earlier.










