Primary Care Doctors Important in Detecting and Managing Childhood Mental Illness
The National Alliance on Mental Illness (NAMI) conducted a survey to determine ways that primary care providers can better communicate with parents about a child’s mental illness. In a news release NAMI executive director Michael Fitzpatrick said, “Most Americans rely on family doctors and pediatricians for early detection of mental illness and in many cases treatment.”
NAMI concluded that primary care providers could play a larger role in detecting mental illness in children. They found that in 63% of families, the first signs of behavioral or emotional problems were evident in children by age 7. More than half of families reported that their primary care physicians were not knowledgeable about mental health treatments. Almost two-thirds of families reported that their primary care providers were not knowledgeable about local resources to support families with mentally ill children.
NAMI’s suggestions for primary care providers included educating themselves about early-onset mental illness and local resources for families, providing screening tools for parents and youth in order to encourage discussion of mental health, emphasizing that mental health is as important as physical health to a child’s wellbeing, asking questions about mental health as a routine part of office visits, and listening to families’ concerns without judgment.
Primary care providers are also encouraged to let families know that there is hope and that they are not alone in facing this difficulty, that mental illness in a child is not the parents’ fault, and that their children have many strengths.
Primary care doctors should also be prepared to: refer a mentally ill child to psychiatrists, psychologists, and other specialists if needed; follow up, including collaborating with other healthcare providers to develop and implement a treatment plan; and encourage patients and their families.
Puberty Occurs at Younger Ages
Experts disagree about the data that show an earlier onset of depression and bipolar disorder in every successive generation since the first World War (this change is called the cohort effect). Nonetheless, it is interesting that so many other medical conditions are increasingly seen in young children. These include asthma, arthritis, obesity, allergy, diabetes, and a host of other conditions. WebMD reported that menarche and the onset of puberty are also occurring at younger ages. Puberty used to be a largely teenage occurrence, and now it occurs in many children as early as age 7.
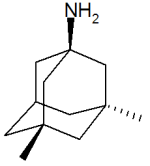
Update: Memantine as an Adjunct to Lamotrigine for Bipolar Depression
Memantine (Namenda), which is approved by the Federal Drug Administration (FDA) for use in Alzheimer’s Dementia, is increasingly being used for other conditions. Some doctors prescribe memantine for hyperactivity and attention problems in attention deficit hyperactivity disorder (ADHD), for obsessive compulsive disorder (OCD), and most recently as an adjunct to lamotrigine in bipolar depression. We wrote about the findings of Amit Anand et al. on the use of memantine and lamotrigine in January. These findings have just been published in Bipolar Disorders. The study indicates that the combination of lamotrigine with memantine brought about a rapid onset and greater magnitude of antidepressant effects than the combination of lamotrigine and placebo. The initial dose of memantine was 5mg/day, which was increased to 20mg/day during the study.
Editor’s Note: The potential mechanism of this effect makes sense. Lamotrigine decreases release of glutamate, and memantine blocks glutamate’s actions at the NMDA receptor. Thus the two together would more efficiently decrease glutamate’s effects.
It is possible that memantine could be effective without effecting the normal functions of glutamate. The drug blocks NMDA glutamate receptors that are situated away from the synapse, while allowing NMDA glutamate receptors at the synapse to fulfill their normal functions that support learning and memory. The blocking of only those receptors outside the synapse (extra-synaptic) could explain why memantine has relatively few side effects.
New Drug Cariprazine May Be Effective in Acute Mania
 Medscape Medical News reported that a new antipsychotic, cariprazine, may be effective in treating acute mania in bipolar I disorder. The drug is produced by Forest Laboratories Inc. and Gedeon Richter Plc.
Medscape Medical News reported that a new antipsychotic, cariprazine, may be effective in treating acute mania in bipolar I disorder. The drug is produced by Forest Laboratories Inc. and Gedeon Richter Plc.
The data showed that patients with acute manic episodes who were treated with cariprazine experienced significant improvements in symptoms compared with patients given placebo, as measured by the Young Mania Rating Scale (YMRS). These improvements, report the companies, were observed as early as day 5 of treatment and at each subsequent time point in the study.
The multicenter, double-blind placebo-controlled parallel group study showed statistically significant improvement in patients receiving cariprazine in each of 2 dosages — 3 to 6 mg/day (-6.1 points, P < 0.001) and 6 to 12 mg/day (-5.9 points, P < 0.001) — as compared with patients receiving placebo.
See here for a history of the research on cariprazine.
Mothers’ SSRI Use May Lead to Increased Risk of Pulmonary Hypertension in Infants
The New York Times summarized findings about the effect of mothers’ antidepressant use on enfants from an article published by Kieler et al. in the British Medical Journal this year.
Researchers have long suspected a link between the use of selective serotonin reuptake inhibitors, or S.S.R.I.’s, and [pulmonary hypertension in babies], but previous studies have been small and inconclusive (with results ranging from there being no link to a six times greater risk).
This research, based on 1.6 million births in Denmark, Finland, Iceland, Norway or Sweden from 1996 to 2007, showed that among women using S.S.R.I.’s, the risk of persistent pulmonary hypertension for infants more than doubled (particularly for use late in pregnancy). It’s still a small risk: 3 in 1000 births, as opposed to 1.2 per 1000 births overall. But it’s a small risk of a serious problem.
Pulmonary hypertension, Dr. Juliette Madan, a pediatrician at the Dartmouth Hitchcock Medical Center explained, is diagnosed when an infant struggles to get enough oxygen into her lungs, and therefore into her bloodstream. The condition can be deadly, although Dr. Madan said that it’s usually treatable — with possible lifelong consequences.
But other research suggests that untreated depression during pregnancy has its own risks, including pre-term birth and low birth weight. Given that, how should a pregnant woman and her doctor weigh the competing risks?
See the New York Times for a discussion on how to balance mother’s health with babies’ health.
Quetiapine May Be an Effective Monotherapy for Bipolar I
 An article published by Weisler et al. last year in the Journal of Clinical Psychiatry suggests that quetiapine may be effective as a monotherapy maintenance treatment for bipolar I disorder. It has previously been shown to work in combination with lithium or divalproex and is approved by the Federal Drug Administration for this combination treatment.
An article published by Weisler et al. last year in the Journal of Clinical Psychiatry suggests that quetiapine may be effective as a monotherapy maintenance treatment for bipolar I disorder. It has previously been shown to work in combination with lithium or divalproex and is approved by the Federal Drug Administration for this combination treatment.
Adult patients diagnosed with bipolar I disorder who were currently or recently in a mood episode received open-label quetiapine in doses of 300-800mg per day for up to 24 weeks. Patients who became stable either remained on quetiapine or were switched to lithium (at doses of 0.6-1.2 mEq/L) or placebo. This double-blind phase of the study continued for up to 104 weeks.
The study began with 2,438 patients, 1,172 of whom made it to the second phase of the trial. On the main outcome measure of time to recurrence of any mood event, both quetiapine and lithium were significantly better than placebo.
Editor’s Note: In the 50% of patients with a recent mood episode who were able to be stabilized on quetiapine monotherapy, those who remained on long-term quetiapine or those who switched to lithium were both much less likely to have subsequent relapses into either depression or mania than those who switched to placebo. Whether Astra-Zeneca, the company that produces quetiapine, will file to gain Federal Drug Administration approval of quetiapine monotherapy for long-term preventive treatment is not known.
Creative People More Likely to Have Mental Illness
According to a large family study of people with severe mental disorders that was published by Kyaga et al. in the British Journal of Psychiatry last year, people with bipolar disorder and siblings of people with schizophrenia or bipolar disorder were much more likely to be working in creative professions than people without severe mental illness.
Kyaga talked to Medscape Medical News about the study:
“I think the study stresses the importance of treating all patients individually, and with the aim of finding the optimal treatment with regards to effectiveness, while minimizing the adverse effects that medication can have on positive aspects of psychiatric disorders,” Dr. Kyaga said.
“We often encounter the suggestion that lithium reduces creativity in patients with bipolar disorder and that adherence therefore is difficult. Now we can say that it is true that bipolar disorder is in fact associated with increased creativity, but we also know from previous research that terminating treatment with lithium in bipolar disorder will, in the long run, disrupt creative behavior,” he continued.
“We therefore need to pay close attention to what patients tell us while being treated, so that we can find a regimen that will work for them to prevent the disastrous consequences of severe psychiatric disorder, while providing them opportunities to uphold their creative behaviors in the long run,” Dr. Kyaga said.
Prenatal BPA Exposure Might Lead to More Hyperactivity, Depression, and Anxiety in Young Children
An article published by Braun et al. in Pediatrics last year suggests that children who were exposed to higher levels of BPA while in the womb exhibited more anxious and depressed behaviors and poorer emotional control and inhibition at age 3. Braun described the implications of this finding to Medscape Medical News:
“At this point, we don’t know what these findings mean in terms of clinical disorders of behavior,” Joe M. Braun, MSPH, PhD, from the Department of Environmental Health, Harvard School of Public Health, Boston, Massachusetts, told Medscape Medical News. “Future studies will need to determine if BPA exposures are associated with clinical behavior disorders,” he said.
BPA is used in a variety of consumer products, including dental sealants, food/beverage containers and linings, medical equipment, and thermal receipts, such as those from ATM machines. Virtually all people in industrialized nations are exposed to the plasticizer.
“People who are concerned about BPA exposure could decrease or eliminate their consumption of canned or packaged foods; they could also avoid contact with thermal receipts,” Dr. Braun said.
Omega-3 Fatty Acids Could Help Treat ADHD in Children
An article by Bloch & Qawasmi published in the Journal of the American Academy of Child and Adolescent Psychiatry last year suggested that omega-3 fatty acids could improve ADHD in children. The effects were milder than the standard pharmacological treatments for ADHD, but given that omega-3s have few side effects, there would be little risk to using them to supplement traditional treatments or in cases where traditional treatments cannot be used.
Editors note: It would also be worth seeing if omega-3s helped mood symptoms too. A meta-analysis we wrote about here suggests that the omega-3 fatty acid EPA or the combination of EPA plus DHA has positive effects on depression in adults.
Fish Oil May Help Prevent Post-Partum Depression
 An article in Time Healthland last year reported that preliminary research shows that women who took fish oil during pregnancy experienced fewer symptoms of post-partum depression than women who did not take fish oil supplements.
An article in Time Healthland last year reported that preliminary research shows that women who took fish oil during pregnancy experienced fewer symptoms of post-partum depression than women who did not take fish oil supplements.
This data has not yet been replicated, but since there are few side effects to taking fish oil supplements, which are high in omega-3 fatty acids, the risk-to-benefits ratio suggests that there is no reason pregnant women shouldn’t take fish oil supplements to decrease the likelihood of depression after delivery.
We have written before about the possible benefits of omega-3 fatty acids.