“Epigenetic Changes After Trauma May Be Adaptive, Contribute to Resilience”
Originally From Psychiatric News Update
In recent years, research throughout the scientific and medical community has suggested a link between trauma and epigenetic changes, chemical modifications that affect gene activity without actually changing the gene’s DNA sequence. The assumption has been that epigenetic changes in the context of trauma are inherently bad, a form of damage that gets passed from generation to generation. But according to Rachel Yehuda, Ph.D., Endowed Professor of Psychiatry and Neuroscience of Trauma at the Icahn School of Medicine at Mount Sinai, these changes may also be adaptations that promote resilience.
“Sometimes the biological changes in response to trauma or intergenerational trauma are there to help deal with the problem of trauma, not compound its effects,” Yehuda said. “The survival advantage of this form of intergenerational transmission depends in large part on the environment encountered by the offspring themselves.”
Yehuda described this phenomenon as a paradox.
“Parental or ancestral trauma may heighten vulnerability to mental health challenges, but epigenetic adaptations may simultaneously facilitate coping mechanisms,” she said. “Trauma increases susceptibility for psychological distress, but also produces adaptations that help us cope with them.”
Yehuda described research she and her colleagues have conducted to tease out how trauma in parents can affect offspring in the context of the biology of posttraumatic stress disorder (PTSD) in Holocaust survivors and their children. As the research unfolded, Yehuda and colleagues found that survivors’ adult children were more likely to have mood disorders, anxiety disorders, and PTSD than Jewish people whose parents did not directly experience the Holocaust. This was especially true of children of Holocaust survivors who had PTSD. The researchers also found that many children of Holocaust survivors had low levels of the stress hormone cortisol, particularly if their parents had PTSD.
Yehuda and colleagues then conducted a series of studies that looked at the role of glucocorticoid receptors — the proteins to which cortisol must bind to exert its effects — and found evidence that these receptors were more sensitive in people with PTSD.
“In practical terms this means that even though someone with PTSD might have lower circulating levels of cortisol in their blood, their cells might react more strongly to the cortisol that is present,” Yehuda said.
Yehuda said that epigenetics provided further insight on the relationship between hypersensitive glucocorticoid receptors, cortisol, and PTSD. She explained the potential role of methylation, which is a chemical reaction in the body in which a small molecule called a methyl group gets added to DNA or DNA-associated proteins.
“Increased methylation generally impedes RNA transcription, whereas less methylation enhances gene expression,” Yehuda said.
In 2015, Yehuda and colleagues conducted a study involving combat veterans who had PTSD and found lower methylation on an important region on the participants’ glucocorticoid receptor gene. The changes were associated with cortisol and glucocorticoid receptor sensitivity in the study participants, suggesting a potential epigenetic explanation for the association between the trauma of combat and PTSD.
Yehuda said that stress-related epigenetic changes may be reversible. For example, one of the studies conducted by her team revealed that combat veterans with PTSD who benefited from cognitive-behavioral psychotherapy showed treatment-induced changes in the methylation of a gene that regulates glucocorticoid receptor sensitivity. Yehuda said that this finding confirmed that healing is also reflected in epigenetic change.
“That we can transform to meet environmental challenge is a superpower. That is resilience,” Yehuda said.” ?
Yehuda then went on to describe the striking and lasting effects of the psychedelics psilocybin and MDMA in trauma and in helping patients confront their fears in a positive and hopeful fashion. These agents which are given with intensive psychotherapeutic support are not yet FDA approved, but preliminary data suggest that they can have dramatic therapeutic effects in trauma and depression. They can help patients change their attitudes to themselves and the world.
In Mice, Knockout of Circadian CLOCK Genes Resembles Mania
Colleen McClung reviewed and extended previous findings of hers that knocking out a gene known as CLOCK in mice could reproduce most aspects of bipolar mania, including symptoms such as hyperactivity; decreased sleep; less depression; more impulsivity, risk taking, and novelty seeking; and increased reward-seeking including substances such as cocaine, alcohol, and sucrose. This syndrome in mice can be reversed by giving the mice lithium and valproate.
Knocking out the CLOCK gene produced an increased firing rate and burst firing of dopamine neurons in the ventral tegmental area (VTA). Localized knockout of the CLOCK gene in the VTA alone also reproduced the increase in dopamine cell firing.
When McClung and colleagues knocked out CLOCK in the medial prefrontal cortex, the normal development of a type of neurons called GABAergic parvalbumin interneurons did not occur in adolescent mice, and in adulthood, certain neural nets did not mature, leading to increases in oxidative stress, mitochondrial and cellular dysfunction, and the behavioral abnormalities that resembled mania. This animal model thus gives insight into how a genetic deficit in circadian rhythm genes in humans could influence the timing of behavioral abnormalities starting in adolescence and lasting through adulthood.
Expectations Can Affect Treatment Efficacy
 A 2017 article by Vanda Faria and colleagues in the journal EBioMedicine reports that when patients with social anxiety disorder were told they were being treated with an active drug, they had a response rate three times higher than patients who were given the same drug but told it was an inactive placebo. The researchers suggest that the way treatments are presented to patients affects whether they work.
A 2017 article by Vanda Faria and colleagues in the journal EBioMedicine reports that when patients with social anxiety disorder were told they were being treated with an active drug, they had a response rate three times higher than patients who were given the same drug but told it was an inactive placebo. The researchers suggest that the way treatments are presented to patients affects whether they work.
In the study by Faria and colleagues, patients with social anxiety were given the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram for nine weeks. Some were told they had received escitalopram, while some were told they had received a placebo. Not only did those who were told they were taking escitalopram see greater reductions in their anxiety, they also showed more connectivity between the posterior cingulate and the amygdala, a region that is crucial to mediating anxiety.
This finding is in line with other research that has found that patients’ thoughts and expectations during treatment can affect the efficacy of that treatment.
Researcher Isaac Marks found that patients with obsessive compulsive disorder (OCD) with fear of contamination who were told to avoid things they feared, such as touching a toilet seat, did not fare any better than those taking placebo pills. However, those taking SSRIs who tried new behaviors like touching a toilet seat learned that they could do so without a major fear response, and their phobias improved.
Several studies have shown that expectations of antidepressant efficacy have a big effect on whether patients with unipolar depression improve after beginning treatment with SSRIs. Bret R. Rutherford and colleagues reviewed findings on expectancy in major depressive disorder in a 2010 article in the journal Current Psychiatry Review.
When patients are presented with a drug and encouraged to believe it will work, they may gain the confidence to try out new behaviors or ways of looking at things, whether that means exploring new social situations for someone with social anxiety, or feeling hopeful and breaking the habit of negative rumination for someone with depression. As the study by Faria and colleagues shows, expectations can even change patterns of brain connectivity.
Studies of repetitive transcranial magnetic stimulation (rTMS), in which electromagnets placed near the scalp stimulate electrical impulses in the brain, have shown that patients with depression who engage in positive thoughts and conversations with their rTMS provider during the stimulation improve more than those who sit passively. If a patient engages in their habitual negative ruminations during rTMS, these might even be cemented by the rTMS-induced release of glutamate and brain-derived neurotrophic factor (BDNF), which are both involved in learning and memory processes and what has been called experience-dependent neuroplasticity.
Thus, a patient’s thoughts and outlook during treatment may be important to the therapeutic outcomes achieved. While expectations may not be sufficient to produce an effect on their own, it does seem that thoughts and behaviors can improve a treatment’s efficacy.
Chronic Fatigue Linked to Low Metabolism
A 2016 article in the journal PNAS suggests that people with chronic fatigue syndrome, also known as myalgic encephalopathy, share a low metabolic profile.
In the study, researcher Robert K. Naviaux and colleagues measured 612 different metabolites in 63 metabolic pathways. They found abnormalities in 20 of these pathways in people with chronic fatigue. Eighty percent of the abnormal measurements were low.
The low metabolic profile resembled a stage of development some worm larvae go through when environmental conditions are harsh. The phase, called dauer, can be brought on by harsh temperatures, low food supply, or pheromones that indicate high population density. It resembles hibernation in some ways, including changes to mitochondrial function. Dauer allows larvae to live for 4 months rather than their normal lifespan of 3 weeks. They can resume normal development when conditions improve.
The authors suggest that chronic fatigue is a metabolic response to environmental stress, and hope to clarify the link between mitochondrial function and the illness.
Lithium May Work by Restoring Dendritic Spines
New research on mice clarifies lithium’s effects on neurons and suggests how it can lead to improved symptoms. Dendrites are the long projections on neurons that seem to reach out to form synapses with other neurons. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. A 2016 article by research Ben Cheyette and colleagues in the journal Molecular Psychiatry reports that in mice with a genetic mutation common to people with autism, schizophrenia, and bipolar disorder, lithium restored healthy numbers of the mushroom-shaped spines. The lithium treatment also reversed symptoms such as lack of interest in social interactions, lack of motivation, and anxiety in the mice.
Cheyette and colleagues first identified a genetic mutation that affects signaling in what is known as the brain’s Wnt pathway. The mutation, while rare, is 80% more common in people with bipolar disorder, autism, and schizophrenia than in people without these disorders.
When the mice were given a similar mutation, they exhibited symptoms such as anxiety, decreased sociability, and lack of motivation. They also had reduced numbers of dendritic spines and impaired Wnt signaling.
Lithium can improve Wnt signaling by blocking an enzyme called GSK-3 beta that impairs the signaling.
Treating the mice with lithium restored their dendritic spines and improved their behavior.
Wnt signaling and dendritic spines may offer the key to lithium’s success in treating a variety of psychiatric disorders in people.
Mysteries Remain in the Relationship Between Inflammation and Depression
At the 2017 meeting of the American College of Psychiatrists, researchers Charles L. Raison and Vladimir Maletic gave a plenary lecture on the role of inflammation in depression. Meta-analyses have confirmed that inflammatory markers including Il-1, Il-6, TNF alpha, and CRP are elevated in about 1/3 of depressed patients. However, Raison and Maletic made the point that anti-inflammatory medications are not for everyone. While patients with elevated levels of CRP at baseline responded to an anti–TNF alpha antibody, patients with low CRP values at baseline actually got worse.
Raison and Maletic cited three studies that have also linked CRP to differential response to traditional antidepressants. In unipolar depression, those with low CRP respond well to selective serotonin reuptake inhibitor (SSRI) antidepressants, while those with elevated blood levels of CRP seem to respond better to a dopamine-active antidepressant such as bupropion or a noradrenergic-active antidepressant such as nortriptyline or the serotonin norepinephrine reuptake inhibitor (SNRI) antidepressant duloxetine. Patients with high inflammation at baseline also seem to respond better to intravenous ketamine and oral doses of omega-3 fatty acids.
Studies of animals have suggested that inflammation throughout the body is implicated in depression. Studies in which rodents are repeatedly defeated by larger animals show that these animals have increased inflammation from lymphocites (a type of white blood cells) in the blood, and monocytes (another type of white blood cells) from the bone marrow and spleen. This inflammation can induce depression-like behaviors in the rodents, which is prevented if the inflammatory mechanisms are blocked. These data suggest that depression is not just in the brain—inflammation from all over the body plays an important role.
Read more
TDCS Can Change Sleep Duration
A German study published in 2016 suggests that transcranial direct current stimulation (tDCS) can affect the duration of a person’s nightly sleep. Lukas Frase and colleagues compared the effects of two different tDCS parameters and a sham stimulation on the sleep patterns of 19 healthy volunteers.
TDCS is a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain.
Bi-frontal anodal stimulation, intended to increase arousal, significantly decreased total sleep time compared to the other two interventions.
Bi-frontal cathodal stimulation, intended to decrease arousal, did not increase total sleep time, possibly because there is a ‘ceiling’ beyond which good sleepers do not sleep longer.
EEG analysis showed that the anodal stimulation did increase arousal, while cathodal stimulation decreased it.
The research increases what is currently known about sleep-wake regulation by showing that total sleep time can be decreased using anodal tDCS. The researchers hope this knowledge can contribute to future treatments for disturbed arousal and sleep.
BDNF in Learning and Memory
Brain-derived neurotrophic factor (BDNF) is involved in various aspects of learning and memory. The DNA for BDNF contains nine different regulatory sites, each of which is involved in different aspects of learning. Researcher Keri Martinovich studied each site by selectively knocking each one out with a genetic manipulation. She found that blocking the e1 site increased acquisition of new learning and recall in mice, while e2 did the opposite. Blockade of e4 had no effect on these memory functions but markedly blocked the process of extinction, which involves a different kind of new learning.
A mouse that learned to associate a particular cue with a shock (a process known as conditioned fear) will stop reacting to the cue after it is presented many times without a shock. This learning that the cue is no longer associated with the shock is referred to as extinction. The animals with e4 blocked in their BDNF did not develop the new extinction learning, and continued to react to the cue as if it were still associated with the shock.
Editor’s Note: These data may have clinical relevance for humans. The anticonvulsant valproate (trade name Depakote), a histone deacetylase inhibitor, selectively increases the e4 promoter site of BDNF and facilitates extinction of conditioned fear, according to research by Tim Bredy et al. published in 2010.
Clinical trails should examine whether valproate could enhance fear extinction in patients with post-traumatic stress disorder (PTSD).
Types of Epigenetic Modifications
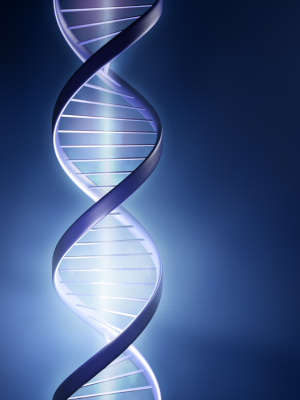 We sometimes refer to epigenetics, a process by which the environment impacts not your inherited genes (based on the DNA nucleotides that encode amino acids to be sequenced in the production of proteins), but how easy it is to activate gene transcription or repress gene transcription.
We sometimes refer to epigenetics, a process by which the environment impacts not your inherited genes (based on the DNA nucleotides that encode amino acids to be sequenced in the production of proteins), but how easy it is to activate gene transcription or repress gene transcription.
There are various epigenetic modifications that can occur. Sometimes acetyl or methyl groups are added to DNA or the histones around which DNA is wound.
1. DNA Methylation (usually repressive)
2. Histone Methylation (usually repressive)
3. Histone Acetylation (usually activating)
4. DNA hydroxymethylation
5. Micro RNAs (si-mRNA) (repressing or activating)
6. Nucleosome remodeling by chromatin regulatory enzymes. If the histone spools around which DNA is wrapped are moved further apart, this is activating. If the histones are moved closer together, this is repressing.
Transgenerational Transmission of PTSD
At a recent scientific meeting, Rachael Yehada showed that PTSD-like traits could be passed transgenerationally. Mothers in New York City who were pregnant on September 11, 2001 and developed post-traumatic stress disorder (PTSD) produced children with low cortisol in their blood (a sign of PTSD). If the fathers had PTSD during the mother’s pregnancy, the children had high cortisol.
These gender-related findings have some parallels in studies of rodents. When a rat pup is separated from its mother for 15 minutes, the mother is overjoyed to see the pup return and licks and grooms it excessively. This maternal overprotection yields an animal with lifelong low cortisol through an epigenetic process. The glucocorticoid receptor gives a feedback message to suppress cortisol, and glucocorticoid receptors are increased in the pups’ brains because of lower methylation of the DNA promoter for glucocorticoid receptors.
If a father has PTSD, there is more methylation of the promoter for glucocorticoid receptors and less expression of them in the forebrain. There is also less feedback suppression of cortisol and the baby exhibits high cortisol.
The methylation of the glucocorticoid receptors in the offspring’s white blood cells is highly correlated (r=0.57, p<0.005, n=23) with methylation in the parent’s white blood cells.