Review Describes Latest Findings on the Mechanisms of Psychedelic Drugs and Their Therapeutic Potential
In a 2021 review article in a special issue of the Journal of Neurochemistry devoted to “Psychedelics and Neurochemistry,” researcher Alaina M. Jaster and colleagues summarized recent findings on psychedelic drugs, including their potential as treatments for psychiatric disorders and the structural changes they produce in the brain. The review article focused on findings in humans and provided background context based on findings in animals, particularly rodents.
In the article, Jaster and colleagues write that psychedelics “have in common a battery of acute (within minutes to hours) effects in humans that include profound changes in processes related to perception, cognition, sensory processing, and mood.” They are not considered to be addictive, and recent research has identified fast-acting and long-lasting therapeutic effects of psychedelics, particularly for the treatment of depression and substance abuse.
While psychedelic drugs interact with the brain in complicated ways, the role of serotonin 5-HT2A receptors seems to be crucial to their effects. Psychedelics have classically been divided into two groups based on their chemical structures: phenethylamines (which include mescaline and its synthetic analog DOI) and tryptamines (which include psilocybin/“magic mushrooms,” DMT/ayahuasca, and ergolines like LSD, which are sometimes separated into a third category). The authors of the review highlight that other substances with different chemical structures that do not fit into this classification can also function as psychedelics. Examples include efavirenz and quipazine, which both activate serotonin 5-HT2A receptors and change rodent behavior in the same way that other psychedelic drugs do. These drugs are providing new directions for research into how psychedelics work at both serotonin 5-HT2A receptors and monoaminergic G protein-coupled receptors (GPCRs).

Rodent studies are often used to investigate how psychedelic drugs work. Rodent behaviors such as ear scratching and head twitching increase when the rodents are given drugs that have psychedelic effects in humans. These behaviors return to normal when rodents are given drugs that function as serotonin 5-HT2A receptor antagonists, preventing the stimulation of these serotonin receptors.
While it has been established that serotonin 5-HT2A receptors play an important role in the hallucinogenic effects of psychedelic drugs, how serotonin receptors are involved in some of the therapeutic effects of psychedelics, such as antidepressant effects and changes to synaptic plasticity, is not yet clear.
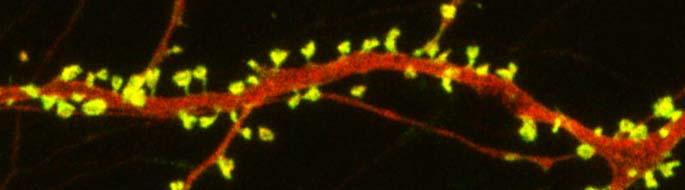
According to the review, “A number of studies in animal models as well as postmortem human brain samples from subjects with depression and controls has provided evidence that mood disorders occur in conjunction with a reduction in the density of dendritic spines, particularly in the frontal cortex.” Dendrites are the projections from the cell bodies of neurons upon which nerve endings from the axons of other neurons synapse. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. The review describes in vitro and in vivo research on mice that suggests that the psychedelics DOI, DMT, and LSD can remodel dendritic spines.
At a recent scientific meeting, researcher Javier González-Maeso, one of the authors of the review, described findings from a recent study of mice given DOI. The structure of the dendritic spines in the prefrontal cortex changed rapidly in these mice. They had also been conditioned to produce a fear response, and the extinction process to get rid of this learned fear was sped up in the mice given DOI. These effects occurred via the serotonin 5-HT2 receptors. The exposure to the psychedelic also affected the regulation of genes involved in synaptic assembly for days, suggesting that epigenetic-induced changes in synaptic plasticity may underlie some of the long-lasting therapeutic effects of psychedelics.
The review also addressed “microdosing,” the recreational practice of consuming small amounts of psychedelics such as psilocybin or LSD, based on the theory that amounts too small to create a hallucinogenic effect may instead produce therapeutic results. The authors find limited data to support microdosing. Most studies in humans and rodents have found no effect or, in the case of one rat study, a worsening of dendritic spine density following microdosing.
Lithium May Work by Restoring Dendritic Spines
New research on mice clarifies lithium’s effects on neurons and suggests how it can lead to improved symptoms. Dendrites are the long projections on neurons that seem to reach out to form synapses with other neurons. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. A 2016 article by research Ben Cheyette and colleagues in the journal Molecular Psychiatry reports that in mice with a genetic mutation common to people with autism, schizophrenia, and bipolar disorder, lithium restored healthy numbers of the mushroom-shaped spines. The lithium treatment also reversed symptoms such as lack of interest in social interactions, lack of motivation, and anxiety in the mice.
Cheyette and colleagues first identified a genetic mutation that affects signaling in what is known as the brain’s Wnt pathway. The mutation, while rare, is 80% more common in people with bipolar disorder, autism, and schizophrenia than in people without these disorders.
When the mice were given a similar mutation, they exhibited symptoms such as anxiety, decreased sociability, and lack of motivation. They also had reduced numbers of dendritic spines and impaired Wnt signaling.
Lithium can improve Wnt signaling by blocking an enzyme called GSK-3 beta that impairs the signaling.
Treating the mice with lithium restored their dendritic spines and improved their behavior.
Wnt signaling and dendritic spines may offer the key to lithium’s success in treating a variety of psychiatric disorders in people.
In Mice, Autism-Like Behavior Connected to Problems Pruning Dendritic Spines
Autism spectrum disorders are associated with developmental abnormalities at excitatory synapses. Dendrites, the branched projections of neurons where electrical signals are passed from one cell to the next, are covered in hundreds to thousands of spines that facilitate the synaptic connections with other neurons. These spines are created and also pruned as part of normal learning and development.
Post-mortem examination of the brains of patients with autism spectrum disorders shows increased density of dendritic spines and less pruning in certain neurons in the temporal lobe. These examinations also show impaired mTOR autophagy. MTOR is a protein that plays a role in cell growth and survival. Autophagy is the normal process by which some components of cells are broken down.
A 2014 study by Guomei Tang et al. in the journal Neuron showed that mice that are genetically altered to have overactive mTOR also have reduced dendritic spine pruning, blockade of autophagy, and increased autism-like behaviors. An immunosuppressant drug called rapamycin inhibits mTOR, and treating the mice with this drug corrected the problems with spine pruning and the autism-like behaviors. (This was not true for mice who had been altered to have another type of autophagy.) Normal spine formation was not affected by the restored pruning ability.
Tang et al. concluded that mTOR autophagy plays an important role in dendritic spine pruning, and that restoring neuronal autophagy can correct synaptic abnormalities and restore normative social behavior in mice with hyperactive mTOR.
Psychiatric Revolution: Changes in Behavior Are Associated with Dendritic Spine Shape and Number
New research shows that cocaine, defeat stress, the rapid-acting antidepressant ketamine, and learning and memory can change the size, shape, or number of spines on the dendrites of neurons. Dendrites conduct electrical impulses into the cell body from neighboring neurons.
Cocaine
Several researchers, including Peter Kalivas at the Medical University of South Carolina, have reported that cocaine increases the size of the spines on the dendrites of a certain kind of neurons (GABAergic medium spiny neurons) in the nucleus accumbens (the reward center in the brain). This occurs through a dopamine D1 selective mechanism. N-acetylcysteine, a drug that can be found in health food stores, decreases cocaine intake in animals and humans, and also normalizes the size of dendritic spines.
Depression
Depression in animals and humans is associated with decreases in Rac1, a protein in the dendritic spines on GABA neurons in the nucleus accumbens. Rac1 regulates actin and other molecules that alter the shape of the spines.
In an animal model of depression called defeat stress, rodents are stressed by repeatedly being placed in a larger animal’s territory. Their subsequent behavior mimics clinical depression. This kind of social defeat stress decreases Rac1 and causes spines to become thin and lose some function. Replacing Rac1 returns the spines to a more mature mushroom shape and reverses the depressive behavior of these socially defeated animals. Researcher Scott Russo has also found Rac1 deficits in the nucleus accumbens of depressed patients who committed suicide. Russo suggests that decreases in Rac1 are responsible for the manifestation of social avoidance and other depressive behaviors in the defeat stress animal model, and that finding ways to increase Rac1 in humans would be an important new target for antidepressant drug development.
Another animal model of depression called chronic intermittent stress (in which the animals are exposed to a series of unexpected stressors like sounds or mild shocks) also induces depression-like behavior and makes the dendritic spines thin and stubby. The drug ketamine, which can bring about antidepressant effects in humans in as short a time as 2 hours, rapidly reverses the depressive behavior in animals and converts the spines back to the larger, more mature mushroom-shape they typically have.
Learning and Extinction of Fear
Researcher Wenbiao Gan has reported that fear conditioning can change the number of dendritic spines. When animals hear a tone paired with an electrical shock, they begin to exhibit a fear response to the tone. In layer 5 of the prefrontal cortex, spines are eliminated when conditioned fear develops, and are reformed (near where the eliminated spines were) during extinction training, when animals hear the tones without receiving the shock and learn not to fear the tone. However, in the primary auditory cortex the changes are opposite: new spines are formed with learning, and spines are eliminated with extinction.
Editor’s Note: It appears that we have arrived at a new milestone in psychiatry. In the field of neurology, changes seen in the brains of patients with strokes or Alzheimer’s dementia have been considered “real” because cells were obviously lost or dead. Psychiatry, in comparison, has been considered a soft science because neuronal changes have been more difficult to see and illnesses were and still are called “mental.” Now that new technologies have made a deeper level of precision, observation, and analysis possible, we know that the brain’s 12 billion neurons and 4 times as many glial cells are exquisitely plastic–capable of biochemical and structural changes that can be reversed using appropriate therapeutic maneuvers.
The changes associated with abnormal behaviors, addictions, and even normal processes of learning and memory now have clearly been shown to correspond with the size, shape, and biochemistry of dendritic spines. These subtle, reproducible changes in the brain and body are amenable to therapeutic intervention, and are now even more demanding of sophisticated medical attention.