Direct Current Stimulation Improves Negative Symptoms of Schizophrenia
 A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
The current study, presented by Ulrich Palm at the 2015 meeting of the Society of Biological Psychiatry, included 20 patients with primarily negative symptoms of schizophrenia, such as thought disorders, poverty of speech, and withdrawal. The patients, who had stable medication regimes for at least three weeks, were randomized to receive either a sham procedure or tDCS with the anode over the left dorsolateral prefrontal cortex and the cathode over the right eye. TDCS stimulation was delivered at a current of 2 mA ten times over two weeks. The patients continued to take their medication and also received functional connectivity magnetic resonance imaging (fcMRI) before and after tDCS treatment.
Two weeks following the stimulation, scores on a scale of positive symptoms (hallucinations and delusions) and negative symptoms of schizophrenia had decreased significantly in those who received tDCS compared to the sham procedure. A measure of negative symptoms was significantly lower among the tDCS group throughout the study period and at the 2-week followup. The fcMRI revealed that those who received tDCS had a deactivated cluster in the brain region that includes the nucleus accumbens, the subgenual cortex, and the striatum.
This study suggests that tDCS is a promising treatment for otherwise difficult-to-treat symptoms of schizophrenia.
Efficacy of Direct Current Stimulation in Major Depression
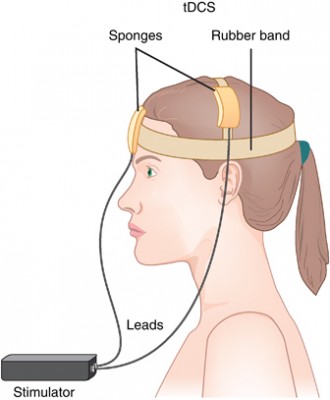 A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
A new meta-analysis presented at the 2015 meeting of the Society of Biological Psychiatry has clarified the efficacy of transcranial direct current stimulation (tDCS) in major depression. TDCS is a treatment in which electrodes deliver a steady low level of electrical stimulation to the brain. The meta-analysis presented by Andre Brunoni and colleagues used individual patient data from six recent studies comparing tDCS treatment to a sham treatment, totaling 289 patients. TDCS treatment was superior to the sham control in terms of antidepressant response (34% to 19%), remission rates (23.1% to 12.7%), and improvement in depression.
After adjusting for confounding factors, the researchers found that patients who had failed to respond to previous treatments were less likely to respond well to tDCS than other patients. They also found that higher doses of tDCS (in terms of current density, duration, and number of sessions) predicted a better response than lower doses.
RTMS for Depression Increases Volume of Specific Brain Regions
Repeated transcranial magnetic stimulation (rTMS) is a treatment for depression in which magnets placed near the skull stimulate electrical impulses in the brain. In a poster presented at the 2015 meeting of the Society of Biological Psychiatry, Martin Lan and colleagues presented results of the first study of structural changes in the brain following rTMS.
In the study, 27 patients in an episode of major depression underwent magnetic resonance brain scans before and after receiving rTMS treatment over their left prefrontal cortices. Lan and colleagues reported that several cortical regions related to cognitive appraisal, the subjective experience of emotion, and self-referential processing increased in volume following rTMS treatment: the anterior cingulate, the cingulate body, the precuneous, right insula, and gray matter in the medial frontal gyrus. The increases ranged from 5.3% to 15.7%, and no regions decreased in volume. More than 92% of the participants showed increased gray matter in all of these regions.
The brain changes were not correlated with antidepressant response to rTMS, but suggest a possible mechanism by which rTMS is effective in some people. Lan and colleagues concluded that rTMS likely had neuroplastic effects in areas of the brain that are important for emotion regulation.
Predictors of Bipolar Disorder in At-Risk Youth
A new longitudinal study of 391 youth at risk for bipolar disorder revealed some predictors of the disorder. The study by Danella M. Hafeman and colleagues was presented at the 2015 meeting of the Society of Biological Psychiatry. The participants were aged 6–18 and each had a parent with bipolar disorder. Over the course of the study, 40 developed an illness on the bipolar spectrum, including 21 who developed bipolar I or II. The participants were assessed for various descriptive characteristics and those who developed bipolar disorder were compared to those who developed major depressive disorder.
The most important predictors of bipolar disorder were parental assessment of internalizing symptoms of anxiety or depression, self-assessment of mood changeability, and self-assessment of hostility. A diagnosis of bipolar disorder not otherwise specified (BP-NOS) was the only predictor of a later diagnosis of bipolar I or II.
Editors Note: These data resemble findings from a 2015 study by David Axelson and colleagues in the American Journal of Psychiatry that used the same cohort of participants. The Axelson study indicated that a categorical diagnosis of a major psychiatric disorder occurred in 74% of the offspring of a bipolar parent compared to about 50% in a control group from the community. Depression, anxiety, attention deficit hyperactivity disorder (ADHD), and oppositional disorders were even more common than bipolar disorder in the at-risk population.
The presence of a major psychiatric diagnosis in about three-quarters of the offspring of a parent with bipolar disorder suggests the importance of early vigilance. One way to track symptoms of depression, anxiety, ADHD, oppositional behavior, and bipolar disorder is to join the Child Network, a secure online platform for rating children’s moods, medications, and side effects. These weekly ratings can be collected longitudinally and printed out to help parents and clinicians assess mood difficulties in their children.
Link Between Childhood Trauma and Difficult Course of Bipolar Disorder Clarified
A collaboration between Norwegian and French researchers led by Bruno Etain has clarified the pathway by which childhood trauma is linked to worse outcomes among people with bipolar disorder. The researchers, who presented their work in a poster at the 2015 meeting of the Society of Biological Psychiatry, replicated earlier findings by this editor (Robert Post) that patients who experienced trauma as a child had a more adverse course of bipolar disorder. Etain and colleagues found a link between childhood trauma and an earlier age of onset of bipolar disorder, rapid cycling, suicide attempts, and cannabis misuse.
The researchers identified more than 550 patients with bipolar disorder, who answered questionnaires about their history of bipolar disorder and childhood trauma. Their DNA was also analyzed, and the researchers found that the effect of childhood trauma on age of onset was mediated by the presence of common genetic variants in proteins related to stress (the serotonin transporter) and immune function (Toll-like receptors). They also found that the traits of mood lability (or moodiness) and impulsivity mediated the effects of trauma on clinical outcomes.
The lasting epigenetic effects of child maltreatment and adversity noted in the above abstract are consistent with a large literature showing more epigenetic effects in these individuals than in controls. While genetics are important, the impact of the environment is also substantial.
N-acetylcysteine Reduces Self-Harm, Restores Amygdala Connectivity in Young Women
 N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
N-acetylcysteine (NAC) is an anti-oxidant nutritional supplement that has been found to reduce a wide range of habitual behaviors, including drug and alcohol use, smoking, trichotillomania (compulsive hair-pulling), and gambling. It also improves depression, anxiety, and obsessive behaviors in adults, as well as irritability and repeated movements in children with autism. A new study suggests NAC may also be able to reduce non-suicidal self-injury, often thought of as “cutting,” in girls aged 13–21.
The open study, presented in a poster by researcher Kathryn Cullen at the 2015 meeting of the Society for Biological Psychiatry, compared magnetic resonance imaging (MRI) scans of 15 healthy adolescent girls to scans of 22 girls who had been engaging in self-injury, both before and after this latter group received eight weeks of treatment with N-acetylcysteine. Doses were 1200 mg/day for the first two weeks, 2400mg/day for the next two weeks, and 3600mg/day for the final four weeks. The girls also reported their self-injury behaviors.
Treatment with NAC reduced the girls’ self-injury behaviors. The brain scans showed that NAC also increased resting-state functional connectivity between the amygdala and the insula. Connectivity in this region helps people regulate their emotional responses. At baseline, the girls who engaged in self-harm had had deficient connectivity between the amygdala, the prefrontal cortex, insula, and the posterior cingulate cortices compared to the healthy girls, and this improved with the NAC treatment.
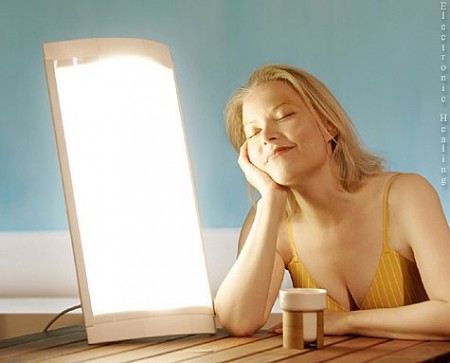
Midday Bright Light Therapy Effective in Bipolar Disorder
A recent study of 93 adults with bipolar disorder suggests that midday bright light therapy can be an effective adjunctive treatment for bipolar depression. The study by Dorothy Sit and colleagues was presented at the 2015 meeting of the Society for Biological Psychiatry. Participants had been diagnosed with bipolar I or II disorder, were in a current episode of depression, and were taking stable doses of mood stabilizing medication. They were randomized to receive either 7000-lux broad spectrum light for 45 to 60 minutes each day for six weeks or 50 lux dim red light. The comparison was dramatic: remission rates were 56.5% among those exposed to the 7000-lux light, and 14.3% among those who were exposed to the dim light. Those who received the bright light also reported better sleep quality and less suicidality.
Editor’s Note: These results are striking and raise the issue of whether midday bright light is more effective than early morning bright light, the usual recommendation for seasonal affective disorder (SAD) and other forms of depression. Until comparative studies are available, using midday light may be the way to go.
Maternal Infection During Pregnancy May Increase Risk of Schizophrenia in Offspring
 There is mounting evidence from animal studies and epidemiological research that an infection during pregnancy may increase the risk of schizophrenia in the offspring. A recent study by Alan Brown and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry used a large dataset from the Finnish Prenatal Study of Schizophrenia to compare medical data from the mothers of 777 people with schizophrenia (630 with schizophrenia and 147 with schizoaffective disorder) to data from the mothers of 777 healthy people.
There is mounting evidence from animal studies and epidemiological research that an infection during pregnancy may increase the risk of schizophrenia in the offspring. A recent study by Alan Brown and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry used a large dataset from the Finnish Prenatal Study of Schizophrenia to compare medical data from the mothers of 777 people with schizophrenia (630 with schizophrenia and 147 with schizoaffective disorder) to data from the mothers of 777 healthy people.
The study’s biobank contained blood samples taken from the mothers in early to mid-pregnancy, which the researchers used to determine the mothers’ levels of C-reactive protein (CRP), an indicator of inflammation. Higher levels of CRP were associated with increased risk of schizophrenia in the offspring. When the researchers analyzed the findings by sex of the offspring, the link between prenatal infection and schizophrenia risk was significant in males, but not females. The effect was also stronger among offspring born after their due date than those born at or before their due date.