A Novel Drug Shows Promise in the Treatment of Negative Symptoms of Schizophrenia

At a recent scientific meeting, Kenneth Koblan, Chief Scientific Officer at Sunovion Pharmaceuticals, Inc. reported on a new drug in development, SEP-363856, and its effects on negative symptoms of schizophrenia.
In both a 4-week double-blind study of participants with acute schizophrenia and in an open (non-blind) 6-month extension study, SEP-363856 was effective on negative symptoms. In the placebo-controlled acute study, those randomized to 50mg or 75mg of the drug showed improvement of moderate effect size in the following symptoms: blunted affect, avolition, anhedonia, asociality, and alogia. In the extension study, which consisted of 26 weeks of treatment with flexible doses (25/50/75 mg/day) of SEP-365846, patients improved further on multiple scales measuring negative symptoms.
SEP-363856 is a novel trace amine receptor 1 (TAAR1) agonist with serotonin 5-HT1A activity. Koblan and colleagues concluded, “These results suggest that activation of the TAAR1 receptor by SEP-363856, in the absence of D2 receptor blockade, may represent a promising approach to the treatment of negative symptoms in schizophrenia.”
Augmentation Strategies for Negative Symptoms of Schizophrenia
In a 2017 article in the journal JAMA Psychiatry, Christoph U. Correll and colleagues reviewed 42 secondary strategies to treat schizophrenia when the primary antipsychotic treatment has an incomplete effect. Many people with schizophrenia show only a limited response to antipsychotic drugs, so additional treatments are often necessary, but currently there are no US Food and Drug Administration guidelines for combination treatment.
Correll and colleagues compiled data from 29 meta-analyses covering 381 individual trials. They found that while the meta-analyses were well done, the quality of the data in the original studies was lacking.
Focusing on Negative Symptoms
However, since the negative symptoms of the illness such as apathy, withdrawal, and blunted emotional response are the hardest to treat, any amount of improvement in this area could be particularly helpful. Read more
Levels of Amino Acid Proline Interact with COMT Genotype to Affect Negative Symptoms
 In a 2016 article, researcher Catherine L. Clelland and colleagues reported that a patient’s levels of the amino acid proline interact with their genetic profile to influence the seriousness of their negative symptoms. Negative symptoms of schizophrenia and bipolar disorder include flat affect and lack of volition and can be some of the hardest symptoms to treat.
In a 2016 article, researcher Catherine L. Clelland and colleagues reported that a patient’s levels of the amino acid proline interact with their genetic profile to influence the seriousness of their negative symptoms. Negative symptoms of schizophrenia and bipolar disorder include flat affect and lack of volition and can be some of the hardest symptoms to treat.
High levels of proline in the central nervous system have been linked to schizophrenia. Proline is a precursor to the neurotransmitter glutamate, and high proline levels have been found to alter glutamate and dopamine signaling in mice. This is one of the factors affecting negative symptoms.
The other factor affecting negative symptoms is the COMT gene. The enzyme catechol-o-methlyl transferase (COMT) metabolizes dopamine in the prefrontal cortex. There are several common versions of the gene for COMT. The most efficient is known as val-158-val, identifying that the gene has two valine amino acids at position 158. People with high proline levels and the val-158-val version of the COMT gene had fewer negative symptoms than people with high proline levels and another version of the gene, val-158-met (indicating one valine and one methionine amino acid at position 158).
Clelland and colleagues hypothesized that high proline levels may actually counteract the dopamine shortages common in the prefrontal cortex in people with the val-158-val genotype of COMT, which is more efficient at breaking down dopamine in this region.
The mood stabilizer valproate increases proline levels. In the study, which was published in Translational Psychiatry, people with schizophrenia and the val-val genotype had fewer negative symptoms when treated with valproate than those with the val-met genotype who received the same treatment.
Schizophrenia: The Importance of Catching It Early
By the time psychosis appears in someone with schizophrenia, biological changes associated with the illness may have already been present for years. A 2015 article by R.S. Kahn and I.E. Sommer in the journal Molecular Psychiatry describes some of these abnormalities and how treatments might better target them.
One such change is in brain volume. At the time of diagnosis, schizophrenia patients have a lower intracranial volume on average than healthy people. Brain growth stops around age 13, suggesting that reduced brain growth in people with schizophrenia occurs before that age.
At diagnosis, patients with schizophrenia show decrements in both white and grey matter in the brain. Grey matter volume tends to decrease further in these patients over time, while white matter volume remains stable or can even increase.
Overproduction of dopamine in the striatum is another abnormality seen in the brains of schizophrenia patients at the time of diagnosis.
Possibly years before the dopamine abnormalities are observed, underfunctioning of the NMDA receptor and low-grade brain inflammation occur. These may be linked to cognitive impairment and negative symptoms of schizophrenia such as social withdrawal or apathy, suggesting that there is an at-risk period before psychosis appears when these symptoms can be identified and addressed. Psychosocial treatments such as individual, group, or family psychotherapy and omega-3 fatty acid supplementation have both been shown to decrease the rate of conversion from early symptoms to full-blown psychosis.
Using antipsychotic drugs to treat the dopamine abnormalities is generally successful in patients in their first episode of schizophrenia. Use of atypical antipsychotics is associated with less brain volume loss than use of the older typical antipsychotics. Treatments to correct the NMDA receptor abnormalities and brain inflammation, however, are only modestly effective. (Though there are data to support the effectiveness of the antioxidant n-acetylcysteine (NAC) on negative symptoms compared to placebo.) Kahn and Sommer suggest that applying treatments when cognitive and social function begin to be impaired (rather than waiting until psychosis appears) could make them more effective.
The authors also suggest that more postmortem brain analyses, neuroimaging studies, animal studies, and studies of treatments’ effects on brain abnormalities are all needed to clarify the causes of the early brain changes that occur in schizophrenia and identify ways of treating and preventing them.
Direct Current Stimulation Improves Negative Symptoms of Schizophrenia
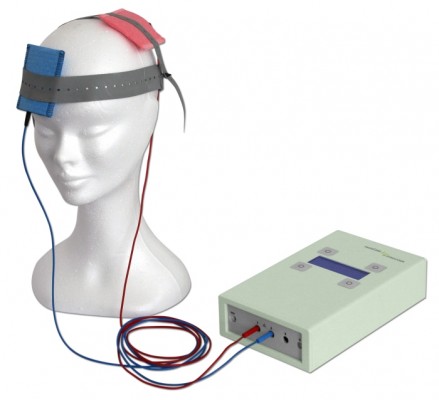 A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
A new double-blind, randomized clinical trial has shown that transcranial direct current stimulation (tDCS) can reduce negative symptoms of schizophrenia. TDCS, a treatment in which an anode and a cathode electrode placed on the skull are used to apply a steady, low-level current of electricity to the brain, has been shown to improve neuroplasticity, such as neuronal remodeling, by depolarizing or hyperpolarizing neurons. People with schizophrenia have neuroplasticity deficits in parts of the cortex, so a few case reports and one previous randomized clinical trial have explored the use of tDCS in schizophrenia.
The current study, presented by Ulrich Palm at the 2015 meeting of the Society of Biological Psychiatry, included 20 patients with primarily negative symptoms of schizophrenia, such as thought disorders, poverty of speech, and withdrawal. The patients, who had stable medication regimes for at least three weeks, were randomized to receive either a sham procedure or tDCS with the anode over the left dorsolateral prefrontal cortex and the cathode over the right eye. TDCS stimulation was delivered at a current of 2 mA ten times over two weeks. The patients continued to take their medication and also received functional connectivity magnetic resonance imaging (fcMRI) before and after tDCS treatment.
Two weeks following the stimulation, scores on a scale of positive symptoms (hallucinations and delusions) and negative symptoms of schizophrenia had decreased significantly in those who received tDCS compared to the sham procedure. A measure of negative symptoms was significantly lower among the tDCS group throughout the study period and at the 2-week followup. The fcMRI revealed that those who received tDCS had a deactivated cluster in the brain region that includes the nucleus accumbens, the subgenual cortex, and the striatum.
This study suggests that tDCS is a promising treatment for otherwise difficult-to-treat symptoms of schizophrenia.