Review: Reconsideration of bipolar disorder as a developmental disorder
Reconsideration of bipolar disorder as a developmental disorder: Importance of the time of onset
Pierre Alexis Geoffroy et al, J Physiology Paris, 2013
Eight admixture studies have demonstrated three homogeneous subgroups of patients with bipolar disorder, identi?ed by their age at onset (early, intermediate and late age at onset), with two cutoff points, at 21 and 34 years.
The early onset group had more: Suicide attempts, rapid cycling, drug and alcohol abuse, psychotic symptoms, panic disorder, OCD, and a positive family history for affective disorder. Early onset illness should be recognized and treated earlier.
Two different subtypes of early onset unspecified bipolar disorder (USBD)
The first subtype is classical BP NOS (Not Otherwise Specified) having all the characteristics of full-blown bipolar disorder except for only having brief durations of mania and responding to conventional treatment. The second is what is now called Temperature and Sleep Dysregulation Disorder (TSDD) and was formerly described by D. Papolos as the Fear of Harm (FOH) syndrome, and requires a different treatment approach.
Clinicians should be alert to unique symptoms in children who might have TSDD as such a diagnosis would lead to a unconventional treatment paradigm. We emphasize the importance of specifically asking parents about evidence of over heating (red face and red ears) and high tolerance for cold (going outside markedly under-dressed) and the presence of fear of sleep and horrific nightmares, as these may lead one to consider the diagnosis of TSDD.
If these two novel aspects (temperature and sleep dysregulation) occur in the presentation of a highly fearful and behaviorally dysregulated child with bipolar-like symptoms, these may lead to the consideration of an unconventional treatment paradigm. It utilizes 1) high dose lithium; 2) clonidine and other practical approaches to achieve cooling and relieve over heating; and 3) ascending doses of intranasal ketamine (as described by Papolos et al 2013; 2018). This may be of considerable clinical importance as a large group of children with this unique presentation respond very poorly to conventional treatments for bipolar disorder and remain highly impaired and dysfunction throughout their childhood and adolescence.
If these children instead are treated with: lithium (to achieve blood levels of 1.0 meq/L or higher); clonidine (0.1- 0.3mg IR and 0.1mg ER at noon and HS) and other practical ways to achieve cooling; followed by ascending intranasal doses of ketamine (starting at 20mg and increasing toward 80-260mg/day, repeated every 2-3 days), marked improvement can be achieved. This occurs in conjunction with ketamine’s positive effects on fear and aggressive behaviors in association with its ability to reduce core body temperature.
We highlight this potential alternative treatment approach as long term positive effects have been achieved with it in open case series (Papolos et al 2013; 2018 ). The efficacy of this treatment approach has not been validated in controlled clinical trials, but we believe wider recognition of the two subtypes of USBD– BPNOS and TSDD,– will lead to more systematic research on treatment. Actively looking for the unique features of TSDD and pursuing its unconventional treatment may lead to long term positive effects in a child previously viewed as having an intractable psychiatric illness.
Gene CACNA1C is Associated with Early-Onset Bipolar Disorder
Several genes have previously been implicated in bipolar illness. In a recent study, researchers at the Mayo Clinic, led by Paul Croarkin, compared variations in three genes (CACNA1C, ANK3, and ODZN) across 69 children aged 6–15 with mania, a 776-person control group from the Mayo Biobank database, and 732 adults with bipolar disorder (some with onset in childhood and adolescence and some with onset in adulthood, also from the Biobank). All participants were Caucasian, to minimize confounding by population stratification. The researchers found that the minor allele of rs10848632 in CACNA1C was associated with childhood onset of bipolar disorder. The haplotype (or sequence of nucleotides) T-G-G-T was the one associated with risk. Genetic risk scores were also associated with early onset of illness.
Editor’s Note: In research by Michael McCarthy and colleagues, CACNA1C has been linked to abnormal circadian rhythms in bipolar disorder and to responsiveness to lithium treatment. Together, these data suggest the importance of studying the calcium channel blocker nimodipine (which blocks calcium influx through CACNA1C) in childhood-onset bipolar disorder. A 1999 case report by Pablo A. Davanzo and colleagues described a teenager with ultra rapid cycling bipolar disorder (multiple mood switches/day) that did not respond to a host of conventional medications, who improved dramatically on nimodipine, reaching remission. This author (Robert M. Post) has also seen confirmed responsivity in adults with rapid cycling bipolar disorder (reported in the 2008 book Treatment of Bipolar Illness: A Casebook for Clinicians and Patients, by Post and Gabriele S. Leverich).
Childhood Onset of Bipolar Illness More Difficult than Adolescent and Adult Onset
Research on early-onset bipolar disorder sometimes lumps childhood-onset in with adolescent onset. Researcher Terence Ketter et al. explored differences in illness among 502 patients at the Stanford Bipolar Disorder Clinic. The 107 patients with childhood onsets (before age 13) had a more difficult course of illness in almost all domains compared to the 238 patients with adolescent onsets (age 13–18) or the 157 patients with illness onset in adulthood (after age 18).
Considered separately, both patients with childhood-onset illness and patients with adolescent-onset illness had more comorbid anxiety disorders, alcohol use disorders, eating disorders, prior suicide attempts, rapid cycling in the prior year, and at least five mood episodes over the course of their lifetimes than those patients whose illness began in adulthood. Patients whose illness began in childhood had higher rates of each of these unfavorable illness characteristics and were more likely to have a first-degree relative with a mood disorder.
These data mirror those from the Bipolar Collaborative Network in which this editor (Robert Post) is an investigator, and the larger STEP-BD network led by Perlis et al. All three suggest that in the US, two-thirds of the bipolar disorder seen in adults begins in childhood and adolescence, with about a quarter beginning before age 13.
Ketter suggests that research should not combine childhood and adolescent onset illnesses, which come with different rates of anxiety, alcohol, and eating disorder comorbidity, rapid cycling, and prior episodes. The statistical relevance of some findings can be diluted when the two groups are combined.
Editor’s Note: However, the primary message is that childhood onset bipolar disorder is a more severe version of the illness that deserves greater attention, treatment, and research so that its course can be made more benign. It is a problem that there are no Federal Drug Administration–approved treatments for children under 10 years of age with bipolar disorder.
Bipolar Illness is Worse in the US than in Germany and the Netherlands
At a symposium celebrating the retirement of Willem Nolen, a researcher who spent 40 years studying unipolar and bipolar disorder, from his position at Groningen Hospital in the Netherlands, this editor (Robert Post) discussed progress in the treatment of bipolar disorder over the past 40 years. Despite the availability of lithium; many new mood stabilizers (carbamazepine, valproate, lamotrigine); and many atypical antipsychotics, all of which are anti-manic and some of which are antidepressant (quetiapine and lurasidone), there is still a very high rate of continued illness and treatment resistance, especially in the US.
In fact, research from the Bipolar Collaborative Network, a treatment research network including sites around the US (one run by this editor) and in Germany and the Netherlands, shows that almost everything about bipolar disorder is worse in the US. Americans have more genetic vulnerability because more of their parents have bipolar disorder, and they are more likely to have environmental vulnerability as a result of childhood adversity. Patients in the US also reported having had more stressors at the onset of their illness and more stressors prior to the last episode they had before entering the network at an average age of 40.
Age at illness onset is much lower in the US than in the Netherlands and Germany. About two-thirds of American patients had onset in childhood or adolescence (under 19 years), while only about one-third of the European patients in this study showed these early onsets.
The course of illness is also more difficult in the US. There is more anxiety, substance abuse, and medical comorbidity, and there are more episodes and more rapid cycling. All this resulted in more US patients than European ones who did not respond to naturalistic treatment in our treatment network despite being prescribed multiple medications.
The implication of these data is that we need a new and more concerted approach to bipolar disorder in the US, beginning with early diagnosis and treatment during childhood and adolescence, instead of the 10- to 15-year average delay that was typical about twenty years ago. The duration of the delay to first treatment with a drug to treat mania or depression was an independent predictor of a worse outcome in adulthood. Early intervention should also include therapy and education.
Family-Focused Treatment (FFT), a method pioneered by researchers David Miklowitz and Kiki Chang, has been shown to be much more effective than treatment as usual in children who are at high risk for developing bipolar disorder because they have a family history of the illness and symptoms of an anxiety or depressive disorder or bipolar not otherwise specified (BP-NOS). In this way it may even be possible to head off the full-blown illness before it starts in those children at highest risk.
Important Reminders from the APA Symposium on Special Topics in Bipolar Disorder
Our editor Robert M. Post served as discussant at a symposium on special topics in bipolar disorder at the 2013 meeting of the American Psychiatic Association. Here are some of the findings that were presented at the symposium.
Michael Gitlin of the University of California, Los Angeles (UCLA) emphasized the importance of treating patients until remission in order to achieve functional recovery and prevent cognitive impairment.
Michael Bauer of Dresden, Germany reviewed data showing that early onset of the illness and long delays to first treatment are important predictors of poor response to treatment.
Mark Frye of the Mayo Clinic discussed the promise of pharmacogenomics to aid in the selection of the best medicine for a given individual (i.e. personalized medicine). Currently the presence of one of a few relatively rare gene variations—HLA-B 1502 (in Asian populations) and HLA-A 3101 (in European populations)—can predict that an individual may develop a severe rash when taking the anticonvulsant carbamazepine. Researcher J. Rybakowski has found that a somewhat common variant in the gene responsible for producing brain-derived neurotrophic factor (the val-66-met allele for proBDNF) is associated with a good response to lithium. This may be explained by the fact that lithium increases BDNF, and this could be crucial in those with the val-66-met allele, which functions less efficiently than the more common and better functioning allele val-66-val.
David Miklowitz, also of UCLA, reviewed data that strongly indicates psychotherapy is effective in the treatment and prevention of bipolar depression. He and Kiki Chang of Stanford University found that family focused therapy (FFT) was effective in treating early syndromes that sometimes lead to bipolar disorder (including depression, anxiety, or BP-NOS) in children at high risk for bipolar disorder because of a family history that includes bipolar disorder in a first degree relative. Yesterday we shared the 8 key ingredients to family focused therapy.
In his discussion, Post emphasized several points from each presentation. Among these was the recommendation by both Gitlin and Bauer that patients use a personal calendar to monitor symptoms and side effects. (We offer an easy download of a personal calendar.)
Post also endorsed Bauer’s emphasis on the need for early intervention, since delay to first treatment is an independent risk factor for a poor outcome in adulthood. (This finding has been replicated in three studies — Franchini et al. in 1999, Post et al. in 2010, and Drancourt et al. in 2012.
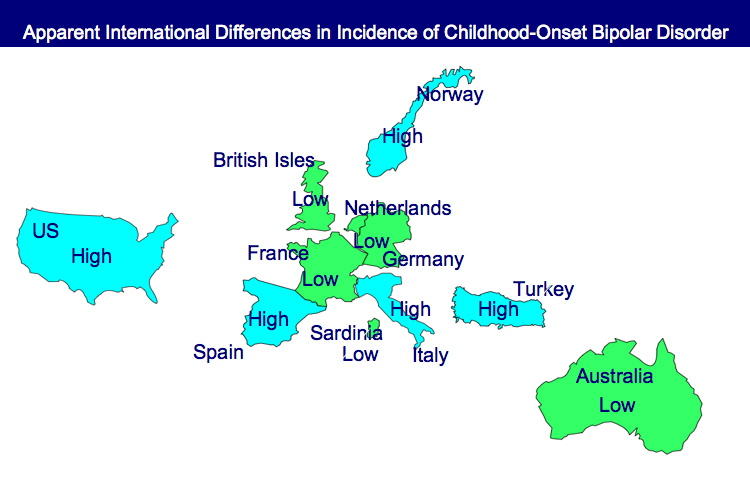
Each of these factors and family focused therapy need greater attention in the US, since Post noted that all aspects of bipolar disorder are more difficult for patients in the US compared to those in Germany, the Netherlands, and many other European countries. About two-thirds of the adults with bipolar disorder in the US had onset of the illness before age 19, while in most European countries, only about one-third of adult patients had an early onset. These data are also consistent with the low incidence of bipolar disorder in children at high risk for the disorder because of a parent with bipolar disorder in studies from the Netherlands, Switzerland, and Germany. In contrast, similar studies of children with at least on parent diagnosed with bipolar disorder in the US (by Chang et al., Nurnberger et al., Wozniak et al., and Birmaher et al.) show a higher incidence of the illness. Canadian studies by Duffy et al. and studies of an isolated Amish community in Pennsylvania by Egeland et al. show a low incidence much like the Europeans.
Given the great need for care of children with signs of bipolar disorder in the US and the shortage of child psychiatrists and pediatricians knowledgeable about bipolar disorder, Post recommended that in the absence of other alternatives, adult psychiatrists of parents with bipolar disorder who have children with the disorder should fill this gap by treating the children themselves. If the child has only early symptoms, family focused therapy as described by Miklowitz above would be recommended.
Tomorrow and Friday we’ll share tables with recommendations for the treatment of parents with bipolar disorder and their children.
Childhood Illness Onset Produces Worse Outcomes
There is more evidence that childhood onset of bipolar illness means a more difficult course of illness. In a study published in World Psychiatry in 2012, Baldessarini et al. pooled data from 1,665 adult patients with bipolar I disorder at seven international sites and compared their family history of bipolar disorder, outcomes, and age of onset. Among these patients, 5% had onset in childhood (age <12 years), 28% during adolescence (12-18), and 53% during a peak period from age 15-25.
Patients who were younger at onset had more episodes per year, more co-morbidities, and a greater likelihood of a family history of the illness. Patients who were older at onset were more likely to have positive functional outcomes in adulthood, like being employed, living independently, and having a family.
Long-term Course of Bipolar Illness is Most Difficult
While the 4 major childhood-onset psychiatric illnesses we discussed this week (bipolar, unipolar, ADHD, and anxiety disorders) show long term difficulties into adulthood in the majority of instances, it appears that the most severely impacted are those with bipolar disorder. These data are also consistent with retrospective data from multiple cohorts of adults with bipolar disorder, which indicate that those whose illness began in childhood fared more poorly in adulthood than those with adult-onset illness. Thus, while there has been a modicum of treatment research in childhood depression and anxiety disorder and a plethora of treatment studies in ADHD, the dearth of treatment studies in children with bipolar disorder is all the more disconcerting.
Bipolar disorder is common, occurring in some 2 to 3% of children and adolescents, and carries a relatively grave prognosis into adulthood in the majority of instances, especially when it is inadequately treated. Virtually all of the investigators in the area of childhood-onset bipolar who presented at the AACAP meeting have pleaded for increased treatment research for bipolar disorder in children, and one can only hope that their message is soon heard.
Studies in Adults Shed Light on the Prevalence of Childhood Bipolar Disorder and the Need for Early Treatment
At the 2011 Pediatric Bipolar Disorder Conference in Cambridge, Massachusetts this past March, Dr. Andrew Nierenberg from Massachusetts General Hospital presented a plenary paper, “What can we learn about bipolar youth from bipolar adults in 2011?”
Since it appears that a substantial number of bipolar adults experience illness onset in childhood, Nierenberg said that a useful approach to treating the illness over the lifetime is to begin treatment in childhood. Early intervention may be more effective and easier to accomplish than treatment much later in the course of illness after multiple pathological psychological, biochemical, and physiological occurrences and interactions have occurred.
Nierenberg’s research was gleaned from reviewing several studies that indicated that a substantial subgroup of bipolar adults had an early age of onset. He included data from his own STEP-BD studies published by Perlis et al. in Biological Psychiatry in 2004 and data from our Bipolar Collaborative Network published by Post et al. in the British Journal of Psychiatry in 2008, as well as a study by Hamshere et al. published in the Journal of Affective Disorders in 2008, a study by Goldstein and Levitt published in the American Journal of Psychiatry in 2006, research by Ortiz et al. and by Bauer et al. both published in Psychiatry Research in 2010, and a study by Baldessarini et al. published in the Journal of Affective Disorders in 2010.
These studies indicate that one-fifth to a quarter of adult outpatients with bipolar disorder experienced illness onset prior to age 13, and one-half to two-thirds of patients experienced their onset in childhood or adolescence, i.e., before age 19.
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more