Lithium Responders and Non-Responders Have Different Neuron Characteristics
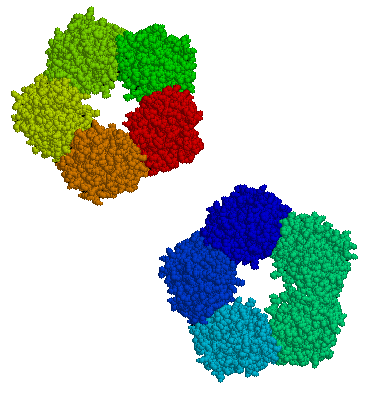
After hyperpolarization (via Wikimedia Commons)
A 2017 study in the journal Molecular Psychiatry suggests that by observing the neurons of a person with bipolar disorder, you can predict whether they will respond to lithium treatment. The drug is effective in approximately 30% of those to whom it is prescribed.
Researchers led by Shani Stern and Renata Santos used stem cell research to analyze neurons from people with bipolar disorder and healthy controls.
People with bipolar disorder shared some neuron features, namely a large, fast after-hyperpolarization (a phase in which the cell’s membrane changes), which is followed by a resting period before the neuron can fire again. The large, fast hyperpolarization in people with bipolar disorder speeds up this cycle, leading to fast and sustained neuron firing. This replicated previous findings by the same researchers, which found that people with bipolar disorder are more sensitive to stimuli. In people with bipolar disorder, the threshold for a neuron to fire drops with each subsequent after-hyperpolarization.
Chronic lithium treatment reduced this hyperexcitability in some patients—and these were the patients who had a good response to lithium treatment.
Among the study participants with bipolar disorder, there were differences in the neuron profiles of those who responded well to lithium versus those who did not.
Stern and colleagues programmed a computer to recognize the electrophysiological features of neurons from lithium responders and non-responders. The computer could then analyze the neurons of a patient whose response to lithium was unknown and predict with a greater than 92% success rate whether that patient had responded well to lithium treatment.
CRP, A Readily Available Marker of Inflammation, Predicts Response To Two Antidepressants
C-reactive protein, or CRP, is a protein found in blood plasma, the levels of which rise in response to inflammation. In a recent study, levels of CRP were able to predict which of two antidepressants a patient was more likely to respond to.
The 2014 article by Rudolph Uher et al. in the American Journal of Psychiatry reported that low levels of CRP (<1 mg/L) predicted a good response to the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) while higher levels of CRP predicted a good response to the tricyclic antidepressant nortriptyline, a blocker of norepinephrine reuptake.
The research was part of the Genome-Based Therapeutic Drugs for Depression (GENDEP) study, a multicenter open-label randomized clinical trial. CRP was measured in the blood of 241 adult men and women with major depressive disorder. In the article the researchers say that CRP and its interaction with medication explained more than 10% of the individual variance in response to the two antidepressants.
If these findings can be replicated with these and similarly acting drugs, it would be a very large step in the direction of personalized medicine and the ability to predict individual response to medications.
Finding Treatments That Work For Each Patient
At a recent scientific meeting, researcher Andrew H. Miller presented data on infliximab, an inhibitor of the inflammatory cytokine TNF alpha that is used to treat rheumatoid arthritis and is being explored for the treatment of depression. As previously reported in BNN Volume 16, Issue 2 from 2012, the drug was not effective overall among the depressed patients, but in a subgroup of patients with high levels of the inflammatory marker CRP, infliximab was highly effective. Miller emphasized that patients do not fail to respond to treatments; it is doctors who fail, or drugs that fail. He explained that there is tremendous heterogeneity in people’s illnesses, and doctors must get better at sorting out what treatments will work for each patient, striving toward personalized therapeutics.
There are many clinical correlates or predictors of nonresponse to antidepressants used in unipolar depression. These include inflammation, obesity, stress in childhood, anxiety disorder comorbidity, substance abuse comorbidity, and medical comorbidity.
Editor’s Note: How do we doctors target these clinical correlates of illness for better therapeutic effects? We are just starting to learn, and until we identify good markers for predicting illness, the best we can do is carry out carefully sequenced clinical trials of medications and therapies with different mechanisms of action.
Patients can assist their physicians and clinicians by engaging in precise, preferably nightly charting of their mood, functioning, medications, life events, side effects, and other symptoms such as anxiety on a personal calendar. Several of these are available for free download, and there are other longitudinal screening instruments, such as the website and app What’s My M3.
A good personal response to a novel treatment or a poor response to an Federal Drug Administration–approved treatment trumps anything that is written in the research literature. The best way to achieve the best outcome is to engage in excellent monitoring of symptoms and side effects that can guide the next steps in therapeutics.
Important Reminders from the APA Symposium on Special Topics in Bipolar Disorder
Our editor Robert M. Post served as discussant at a symposium on special topics in bipolar disorder at the 2013 meeting of the American Psychiatic Association. Here are some of the findings that were presented at the symposium.
Michael Gitlin of the University of California, Los Angeles (UCLA) emphasized the importance of treating patients until remission in order to achieve functional recovery and prevent cognitive impairment.
Michael Bauer of Dresden, Germany reviewed data showing that early onset of the illness and long delays to first treatment are important predictors of poor response to treatment.
Mark Frye of the Mayo Clinic discussed the promise of pharmacogenomics to aid in the selection of the best medicine for a given individual (i.e. personalized medicine). Currently the presence of one of a few relatively rare gene variations—HLA-B 1502 (in Asian populations) and HLA-A 3101 (in European populations)—can predict that an individual may develop a severe rash when taking the anticonvulsant carbamazepine. Researcher J. Rybakowski has found that a somewhat common variant in the gene responsible for producing brain-derived neurotrophic factor (the val-66-met allele for proBDNF) is associated with a good response to lithium. This may be explained by the fact that lithium increases BDNF, and this could be crucial in those with the val-66-met allele, which functions less efficiently than the more common and better functioning allele val-66-val.
David Miklowitz, also of UCLA, reviewed data that strongly indicates psychotherapy is effective in the treatment and prevention of bipolar depression. He and Kiki Chang of Stanford University found that family focused therapy (FFT) was effective in treating early syndromes that sometimes lead to bipolar disorder (including depression, anxiety, or BP-NOS) in children at high risk for bipolar disorder because of a family history that includes bipolar disorder in a first degree relative. Yesterday we shared the 8 key ingredients to family focused therapy.
In his discussion, Post emphasized several points from each presentation. Among these was the recommendation by both Gitlin and Bauer that patients use a personal calendar to monitor symptoms and side effects. (We offer an easy download of a personal calendar.)
Post also endorsed Bauer’s emphasis on the need for early intervention, since delay to first treatment is an independent risk factor for a poor outcome in adulthood. (This finding has been replicated in three studies — Franchini et al. in 1999, Post et al. in 2010, and Drancourt et al. in 2012.
Each of these factors and family focused therapy need greater attention in the US, since Post noted that all aspects of bipolar disorder are more difficult for patients in the US compared to those in Germany, the Netherlands, and many other European countries. About two-thirds of the adults with bipolar disorder in the US had onset of the illness before age 19, while in most European countries, only about one-third of adult patients had an early onset. These data are also consistent with the low incidence of bipolar disorder in children at high risk for the disorder because of a parent with bipolar disorder in studies from the Netherlands, Switzerland, and Germany. In contrast, similar studies of children with at least on parent diagnosed with bipolar disorder in the US (by Chang et al., Nurnberger et al., Wozniak et al., and Birmaher et al.) show a higher incidence of the illness. Canadian studies by Duffy et al. and studies of an isolated Amish community in Pennsylvania by Egeland et al. show a low incidence much like the Europeans.
Given the great need for care of children with signs of bipolar disorder in the US and the shortage of child psychiatrists and pediatricians knowledgeable about bipolar disorder, Post recommended that in the absence of other alternatives, adult psychiatrists of parents with bipolar disorder who have children with the disorder should fill this gap by treating the children themselves. If the child has only early symptoms, family focused therapy as described by Miklowitz above would be recommended.
Tomorrow and Friday we’ll share tables with recommendations for the treatment of parents with bipolar disorder and their children.