Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry.
Compared with the patients in Europe, patients from the US sites had a significantly increased incidence of early onset bipolar disorder, positive family history of unipolar or bipolar affective illness in first-degree relatives, psychosocial adversity, anxiety and substance abuse comorbidities, more than 20 prior episodes, and rapid cycling (four or more episodes) in the year prior to Network entry. Most of these factors are associated with a more difficult course of illness. In addition to these self-reported assessments of the prior course of illness, we also found that fewer patients from the US entered the Network in a well state (and maintained that well state for six months), and more patients from the US who entered the Network ill were nonresponders to naturalistic treatment.
The geographical differences in outcomes appeared despite use of approximately equal numbers of medications, although there were some qualitative differences in medication use noted on the two continents. Patients in Europe were administered more lithium and typical antipsychotics as well as benzodiazepines, while those in the US were treated more often with valproate, atypical antipsychotics, and unimodal antidepressants. Aside from differences in prescribing practices, patients treated in Europe with lithium or the atypical antipsychotics had significantly more positive long-term outcomes than those treated with these same drugs in the US, and there were nonsignificant trends in the same direction for many other drugs.
Assortative mating
When we examined the incidence of a positive family history of affective illness in the parents of the patients in the Network, among US patients there was a greater incidence not only of one parent having bipolar disorder, but also of both parents having an affective disorder. This latter effect is referred to as assortative mating, because it suggests that patients with unipolar and bipolar illness select partners who also have mood disorders or are vulnerable to developing them.
It is not clear why there is an increased positive parental history of disorder in the US compared with Europe and an increased incidence of assortative mating, but these genetic and familial risk factors could be associated not only with the earlier onset of illness in the US, but also with the more pernicious course of bipolar illness in the US. Ascertaining the mechanisms that lead to the more adverse illness course and outcome in the US might shed light on clinical and public health measures that could make the illness more benign. While it appears difficult to do much about the earlier age of onset of illness in the US at present, the delay to first treatment appears to be a risk factor that could be reduced with greater attention to the public health consequences.
Early onset bipolar illness and treatment delay are risk factors for a poor outcome in adulthood
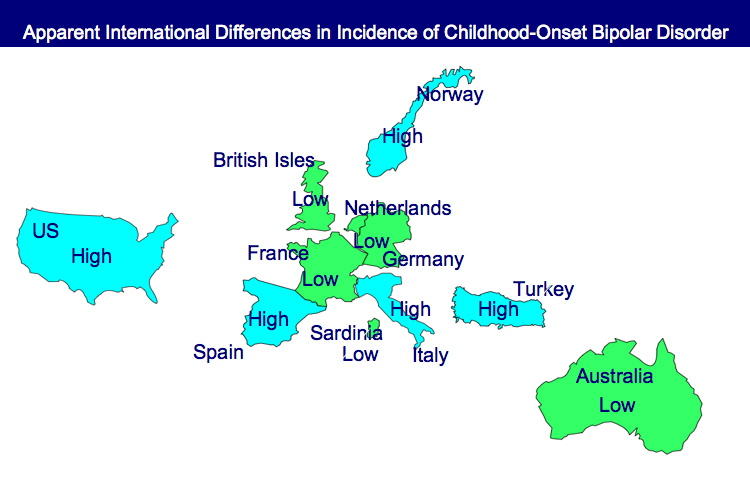
In 2008 we published research that there was a greater incidence of early onset illness (prior to age 13) in the US (22% of people with bipolar illness) than in Europe (2%), and that delays to first treatment for the illness were highly inversely correlated with earlier age of onset.
More recent data showing that early onset bipolar illness and treatment delay are risk factors for a poor outcome in adulthood raise the possibility that earlier intervention in the illness in the US could lead to a less severe course of illness and a better long-term outcome.
The duration of the treatment delay from illness onset to first treatment for mania or depression was an independent correlate of poor outcome upon followup among adults in the Network (average age 42).
Those with the longest delays to first treatment experienced greater amounts and severity of depression, more episodes, and less time euthymic compared with patients with shorter treatment delays.
These data published this year in the Journal of Clinical Psychiatry now parallel a robust literature that the duration of the untreated interval (DUI) is a poor prognosis factor for schizophrenia as well.
Comments
Leave a Reply