Genetic Risk Factors for Onset of Bipolar Disorder
A Genetic Risk Factor For Bipolar Disorder: The CACNA1C Gene
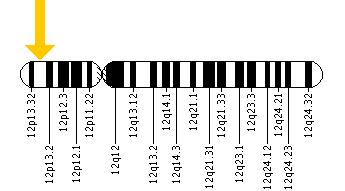
In an abstract presented at the 5th Biennial Conference of the International Society for Bipolar Disorders, Sophia Frangou reported on the CACNA1C polymorphism, a genetic variation that has been associated with the risk of developing bipolar disorder in several genome-wide association studies that search for links between genes and illnesses. Frangou found that those people with the genetic variation had increased volume in some parts of the brain, including the right hypothalamus and the right amygdala, and decreased volume in others, including the putamen, as well as alterations in the functional connectivity of different cortical areas.
These data may be related to findings that calcium influx may play a role in bipolar disorder. In people with the genetic variation, the risk allele binds to a subunit of the voltage-dependent calcium channel, which modulates the influx of calcium from the outside to the inside the neuron.
Increased amounts of calcium are consistently found in the white cells and platelets of patients with bipolar disorder compared to controls. Moreover, the drug nimodipine, a dihydropyridine L-type calcium channel blocker, is effective in the prevention of manic and depressive episodes in a subgroup of patients, particularly those with cycling patterns that are ultra-rapid (4+ episodes per month) or ultradian (including a mood switch within a 24-hour period 4+ times per month). A large randomized study of patients with bipolar disorder presented by H.R. Chaudhry at the 2010 meeting of the Society of Biological Psychiatry also found that while lithium was associated with a 50% response rate, the combination of lithium and nimodipine was associated with a 73% response rate, again suggesting the additional efficacy of blocking L-type calcium channels.
Immune Abnormalities May Predict Onset of Bipolar Disorder in Children at High Risk
At the 5th Biennial Conference of the International Society for Bipolar Disorders E. Mesman discussed connections between immunity and bipolar disorder. Mesman and colleagues followed offspring of parents with confirmed bipolar disorder for 12 years and compared them to children in the general population. In the children of bipolar parents they found higher levels of immune markers called cytokines (PTX3 and sCD25) in circulating monocytes, a type of white blood cell. In the children of bipolar parents they also found a high inflammatory setpoint in the monocytes. T-effector and T-regulatory cells were also different in the offspring of bipolar parents.
While these findings were present in children who had already become ill with bipolar disorder, they were also present in those who had yet to experience a mood disorder, suggesting that these immune and inflammatory markers may ultimately be an important risk marker for the onset of bipolar disorder.
Editor’s Note: These are among the first studies suggesting that immune and inflammatory abnormalities may precede the onset of bipolar disorder. Many studies have shown that patients with active bipolar disorder show more inflammation, including increases in inflammatory markers interleukin 1 (IL-1), interleukin 6 (IL-6), C reactive protein (CRP), and tumor necrosis factor alpha (TNFa). The new data are of considerable importance not only because inflammation could serve as a marker of illness onset, but also because inflammation could become a potential target for therapeutics (i.e. using anti-inflammatory and immune-suppressing agents to treat bipolar disorder).