Inflammation Associated with Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Katherine E. Burdick and colleagues at Brigham and Women’s Hospital and Harvard Medical School reported that in 240 patients with bipolar disorder who were not currently having a manic or depressive episode, markers of inflammation were associated with cognitive deficits.
Inflammation was associated with cognitive deficits in general, and there were also some relationships between specific inflammatory markers and types of cognitive processing. They found that the inflammatory markers TNF-alpha, TNFR1, and TNFR2 influenced cognitive flexibility. The inflammatory marker VEGF influenced reward processing, while IL-6/IL-6r influenced spatial processing. IL-1beta and IL-1RA influenced social cognition.
Burdick and colleagues found it was important to include both primary and secondary mediators of inflammation in their research “as the effects of the primary pro-inflammatory cytokines can be blocked by a number of decoy receptors and soluble antagonists.” Elevations in these can provide additional information about the function of the immune system.
Editor’s Note: Targeting inflammation with the anti-inflammatory treatments minocycline and celecoxib has been shown to improve depression. Now the role of anti-inflammatory drugs in improving cognition deserves further attention.
An Inflammatory State Impedes Treatment for Bipolar Disorder
 A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
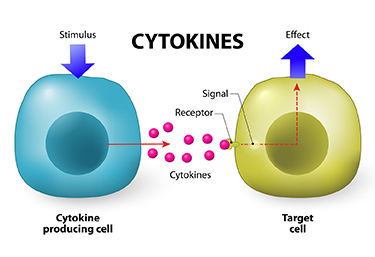
Researcher Francesco Benedetti and colleagues report that high levels of inflammatory cytokines (a type of small proteins) predicted a worse response to treatment with sleep deprivation and light therapy for bipolar depression. This treatment typically brings about a rapid antidepressant response.
Benedetti and colleagues measured 15 immune-regulating compounds in 37 patients who were experiencing an episode of bipolar depression and 24 healthy volunteers. Among those participants with bipolar disorder, 84% had a history of non-response to medication. Twenty-three of the 37 patients, or 62%, responded to the sleep deprivation/light therapy combination. Those who did not had higher levels of five cytokines: interleukin-8, monocyte chemoattractant protein-1, interferon-gamma, interleukin-6, and tumor necrosis factor-alpha.
Body mass index was correlated with cytokine levels and also reduced response to the treatment.
The finding supports a link between the immune system and mood disorders. Evaluating a patient’s level of inflammation may, in the future, allow doctors to predict the patient’s response to a given therapy. Patients with high levels of inflammation might benefit most from treatments that target their immune system.
Early Life Stressors Lead to Lifetime Increase in Inflammation in Mice
Stressors in early life can contribute to the risk of developing mood disorders. Given that many treatments for mood disorders work by blocking the serotonin 5-HT transporter, Nicole Baganz and colleagues designed a study to see whether an early life stressor, in this case maternal separation, would affect immune processes that in turn affect serotonin signaling.
In this study as in many before it, mice that were removed from their mothers exhibited behaviors that resembled human anxiety and depression. They were also found to have elevated messenger RNA for several inflammatory cytokines (including IL-1beta and IL-6) in their brain and blood. Mice that had a gene for the interleukin-1 receptor (IL-1R) removed exhibited neither the depressive behavioral effects nor the changes in cytokine levels following maternal separation, showing that the IL-1R gene plays a necessary role in the signaling process that leads to this type of depression. Levels of the stress hormone corticosterone in the blood did not differ in the mice with and without the IL-1R gene.
The researchers concluded that early life stressors can cause lifelong changes in inflammatory cytokine levels in mice.
Abnormal Levels of Cytokines Found in Brains of Suicide Victims
Cytokines are chemical messengers that send signals between immune cells and between the immune system and the central nervous system. Their levels in blood are considered a measure of inflammation, which has been implicated in depression and stress. A new study by Ghanshyam Pandey and colleagues reported increased levels of cytokines in the brains of people who committed suicide. In the prefrontal cortices of people who died by suicide, there were significantly elevated levels of the inflammatory cytokines IL-1 beta, IL-6 and TNF-alpha compared to the brains of normal controls. There were also lower levels of protein expression of the cytokine receptors IL-1R1, IL-1R2 and IL-1R antagonist (IL1RA) in the suicide brains compared to controls.
The researchers concluded that abnormalities in proinflammatory cytokines and their receptors are associated with the pathophysiology of depression and suicide. This research provides direct confirmation of the indirect measures of inflammation observed in the blood of depressed patients compared to controls.
Depression May Not Be All in Your Head
 Repeated social defeat stress (when an intruder mouse is repeatedly threatened by a larger mouse defending its home territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit depression-like behaviors such as social avoidance and loss of interest in sucrose. Georgia Hodes, a researcher at Mount Sinai School of Medicine, reported at a recent scientific meeting that repeated defeat stress–induced behavior was blocked when IL-6, an inflammatory cytokine released by white blood cells in the blood, was inhibited. The central nervous system did not appear to be involved.
Repeated social defeat stress (when an intruder mouse is repeatedly threatened by a larger mouse defending its home territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit depression-like behaviors such as social avoidance and loss of interest in sucrose. Georgia Hodes, a researcher at Mount Sinai School of Medicine, reported at a recent scientific meeting that repeated defeat stress–induced behavior was blocked when IL-6, an inflammatory cytokine released by white blood cells in the blood, was inhibited. The central nervous system did not appear to be involved.
Interestingly, mice with more white blood cells and more IL-6 release at baseline (prior to the social defeat stress) were more likely to show the defeat-stress depressive behaviors.
Editor’s Note: The higher number and greater reactivity of white blood cells seen in these mice could be a clinical marker of vulnerability to defeat stress, and such findings are worthy of study in human depression. White blood cells are critical to fighting infection and sometimes their overactivity can contribute to inflammation. In meta-analyses, a subgroup of depressed patients consistently show elevated inflammatory markers (including IL-1, IL-6, TNF alpha, and CRP), and it remains to be seen whether these markers of inflammation are generated in the central nervous system or come from white blood cells in the blood, and whether their targeted suppression could be a new route to antidepressant effects (as in the study of defeat stress in mice).
Inflammation and Anti-Inflammatories in Depression
Depression is often associated with increases in markers of inflammation in blood, which include IL-1, IL-6, TNF-alpha, and CRP. Risk factors for increased inflammation include stress, obesity, a diet high in omega-6 fatty acids, sedentary lifestyle, social isolation, low socio-economic status, smoking, and being female. Treatments such as lithium, other mood stabilizers, and antidepressants can all have anti-inflammatory effects.
At the International Congress of Neuropsychopharmacology in 2012, researcher Michael Berk reviewed data on inflammation in depression. Berk shared prospective data that in the general population, people whose levels of CRP fall within the highest third have the highest risk for a new onset of depression over the next 9 years, while those with CRP values in the lowest third (indicating low inflammation) had the least likelihood of becoming depressed.
Drugs with more direct anti-inflammatory properties are beginning to be studied in unipolar depression with some success. In a trial by Abbasi et al. published in the Journal of Affective Disorders in 2012, the anti-inflammatory COX-2 inhibitor celecoxib (Celebrex) when added to the selective serotonin reuptake inhibit (SSRI) sertraline (Zoloft) had better antidepressant effects than the addition of placebo.
Sepaujnia et al. reported in Neuropsychopharmacology in 2012 that an anti-diabetes drug that also has anti-inflammatory properties, pioglitazone (Actos), also beat placebo in depression.
Laan et al. reported in the Journal of Clinical Psychiatry that the same was true of acetylsalicylic acid (ASA or aspirin).
Finally, Berk summarized data that the class of cholesterol-lowering drugs called statins are also able to decrease CRP and improve or prevent depression. Epidemiological data by Pasco et al. published in Psychotherapy and Psychosomatics showed that subjects without depression were less likely to develop a new onset of depression if they were treated with statins compared to those who were not. Stafford et al. reported in the Journal of Clinical Psychiatry in 2010 that patients taking statins had a 79% decreased likelihood of depression at 9 months of follow-up. A third study in Sweden showed that simvastatin, a lipophilic (fat-soluble) drug that can readily enter the brain, decreases the incidence of depression more than some of the non-lipophilic statins.
Moreover, a meta-analysis by O’Neil et al. reported that overall, statins had positive effects on mood.
Editor’s Note: All these data come from studies of unipolar depression, so one must consider how relevant they are to bipolar depression. They may be pertinent, since elevated inflammatory markers have consistently been reported in bipolar depression. However, this cannot be assumed until appropriate studies are performed. (As usual, research in bipolar depression lags far behind that in unipolar depression.)
Preliminary uncontrolled retrospective data from one study did suggest that those treated with lithium plus aspirin did better than those on lithium and no anti-inflammatory.
Thus it may make sense for unipolar and bipolar depressed patients with risk factors for heart disease such as a positive family history of heart disease and elevated cholesterol and triglycerides to discuss with their doctors the possibility of starting statin treatment earlier rather than later. This is because depression itself is a major risk factor for heart disease, so statins might lower risk both by their approved indication of lowering cholesterol and by their apparent ability to help fend off new episodes of depression.
A more complicated issue would be the question of when, if at all, to use primary anti-inflammatory drugs in the adjunctive treatment of unipolar or bipolar depression. Read more
Immune Mechanisms Are Important to the Emergence of Defeat Stress–Induced Depressive Behaviors
At a recent scientific meeting, researcher Georgia E. Hodes presented evidence that in mice, the immune system may play a role in behaviors that resemble human depression. Repeated social defeat stress (when an intruder mouse is threatened by a larger mouse defending its territory) is often used as a model to study human depression. Animals repeatedly exposed to social defeat stress start to exhibit social avoidance and lose interest in sucrose. Hodes et al. determined that interleukin 6 (IL-6), an inflammatory cytokine, or signaling molecule, secreted into the blood was crucial to these behaviors. When the researchers injected mice with antibodies that block the effects of IL-6, or when they irradiated the mice’s peripheral immune system to prevent the formation of IL-6, the depressive behaviors did not emerge following defeat stress.
Editor’s Note: There are increasing data that immunological and inflammatory mechanisms play a role in human affective disorders, and these preliminary data raise the possibility that blocking some immune mechanisms more directly in humans could be a novel therapeutic approach to explore in the future.
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more