Inflammation Associated with Cognitive Deficits
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Katherine E. Burdick and colleagues at Brigham and Women’s Hospital and Harvard Medical School reported that in 240 patients with bipolar disorder who were not currently having a manic or depressive episode, markers of inflammation were associated with cognitive deficits.
Inflammation was associated with cognitive deficits in general, and there were also some relationships between specific inflammatory markers and types of cognitive processing. They found that the inflammatory markers TNF-alpha, TNFR1, and TNFR2 influenced cognitive flexibility. The inflammatory marker VEGF influenced reward processing, while IL-6/IL-6r influenced spatial processing. IL-1beta and IL-1RA influenced social cognition.
Burdick and colleagues found it was important to include both primary and secondary mediators of inflammation in their research “as the effects of the primary pro-inflammatory cytokines can be blocked by a number of decoy receptors and soluble antagonists.” Elevations in these can provide additional information about the function of the immune system.
Editor’s Note: Targeting inflammation with the anti-inflammatory treatments minocycline and celecoxib has been shown to improve depression. Now the role of anti-inflammatory drugs in improving cognition deserves further attention.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.
Anti-Inflammatory Treatments Improve Depression
Inflammation can interfere with the balance of neurotransmitters in the brain, making antidepressants less effective. Anti-inflammatory treatments (such as those used to treat rheumatoid arthritis) may help. In a 2016 meta-analysis published in the journal Molecular Psychiatry, researchers led by Nils Kappelmann analyzed the results of 20 clinical trials of chronic inflammatory conditions where depressive symptoms were also recorded. In a subset of 7 clinical trials that compared anti-inflammatory treatment to placebo, they found that anti-inflammatory treatment improved depressive symptoms significantly compared to placebo.
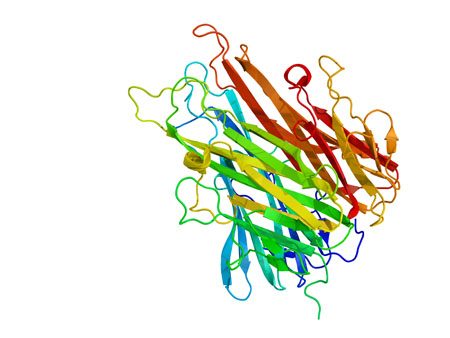
The anti-inflammatory drugs studied most often targeted the inflammatory marker tumor necrosis factor (TNF) alpha using an antibody. Some of the anti-inflammatory drugs that improved depressive symptoms were adalimumab, etanercept, infliximab, and tocilizumab.
The researchers also found that those participants with the most inflammation when they began treatment saw the largest improvement in their depression after taking anti-inflammatory treatments.
Kappelmann and colleagues suggest that inflammation may cause depression, and that anti-inflammatory drugs may be useful in the treatment of depression in people with high inflammation.
Psychotherapy Improved Depression, Reduced Inflammation
A recent study shows that psychotherapy can not only improve depression symptoms, but may also reduce the inflammation that often accompanies them.
Researcher Jean Pierre Oses and colleagues randomly assigned participants with depression to receive Supportive-Expressive psychodynamic therapy, which is designed to help patients understand conflictual relationship patterns, or an alternative therapy. Among the 47 participants who received Supportive-Expressive therapy, depression improved significantly after 16 sessions, and blood levels of the inflammatory markers interleukin-6 and TNF alpha also dropped.
The research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Meta-Analysis Shows Inflammation is Common in Unipolar Depression, Bipolar Depression, and Schizophrenia
In a symposium at the 2016 meeting of the Society of Biological Psychiatry, Mark Hyman Rapaport described the results of his research group’s meta-analysis of studies comparing levels of inflammation in the blood of people with unipolar depression, bipolar depression, and schizophrenia. Rapaport and colleagues determined that people acutely ill with any of the three illnesses showed abnormally high levels of certain inflammatory proteins. These included: interleukin-1beta, interleukin-6, TNF alpha, and c-reactive protein. Those who were chronically ill showed elevations in interleukin-6.
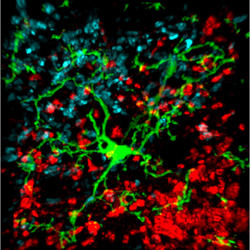
These data are consistent with increasing evidence that inflammation also occurs in the brain. Brain inflammation can be observed by measuring translocator protein binding, a measure of brain microglial activation, using positron emission tomography (PET) scans.
Brain Inflammation Found in Autopsy Studies of Teen and Adult Suicides
Suicide and depression have both been linked to elevated levels of inflammatory cytokines in the blood and cerebrospinal fluid. A recent study finds that these inflammatory markers are also elevated in the brains of teens and depressed adults who died from suicide.
In autopsy studies, researcher Ghanshyam N. Pandey measured levels of the inflammatory cytokines interleukin-1beta, interleukin 6, and TNF-alpha in the brains of teen suicide victims, and compared these to the brains of teens who died from other causes. Pandey also measured levels of interleukin-1beta, interleukin 6, interleukin 8, interleukin 10, interleukin 13, and TNF-alpha in the prefrontal cortex of depressed adult suicide victims and compared them to levels in adults who died of other causes.
There were abnormalities in the inflammatory markers in the brains of those who died from suicide compared to their matched controls. The suicide victims had higher levels of interleukin-1beta, interleukin 6, and TNF-alpha than the controls. Among the adults, levels of the anti-inflammatory cytokine interleukin 10 were low in the suicide victims while levels of Toll-like receptors (TLR3 and TLR4), which are involved in immune mechanisms, were high.
Brain inflammation has also been observed in positron emission tomography (PET) scans of depressed patients, where signs of microglial activation can be observed. Elevated inflammatory cytokines are also found in the blood of some people with bipolar disorder, depression, and schizophrenia.
Pandey presented this research at the 2016 meeting of the Society of Biological Psychiatry.
Inflammation Linked to Non-Response to Antidepressants
In a symposium on inflammation’s role in psychiatric disorders at the 2016 meeting of the Society of Biological Psychiatry, researcher Carmine Pariante reviewed the considerable literature indicating that major depression is often associated with measures of inflammation. Depression has been linked to elevated blood levels of the inflammatory proteins interleukin-1, interleukin-6, TNF alpha, and c-reactive protein, with about one-third of depressed patients having an elevated level of at least one of these proteins. People with elevated inflammatory markers are also less likely to respond to traditional antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Pariante reported that in depressed people, interleukin-6 is also elevated in cerebrospinal fluid in addition to blood, suggesting that inflammation in depression extends to the central nervous system. Increased secretion of interleukin-6 has been linked to depressive behaviors in mice exposed to stress.
There is some hope that anti-inflammatory treatments can help patients who do not respond to traditional antidepressant treatment. Some anti-inflammatory medications that may eventually be used to treat depression with inflammation include the COX-1 inhibitor aspirin, the COX-2 inhibitor celecoxib (Celebrex), or the antibiotic minocycline. Each of these approaches gained some support in preliminary clinical trials, but it has not yet been established that these anti-inflammatory treatments produce a better response in people with elevated inflammatory markers.
Blood and Now Brain Inflammation Linked to Depression
 There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
Common inflammatory markers that have been linked to depression include IL-6, TNF-alpha, and c-reactive protein. At the meeting, Meyer reviewed the findings on each of these. Twelve studies showed that IL-6 levels are elevated in the blood of patients with depression. Four studies had non-significant results of link between IL-6 and depression, and Meyer found no studies indicating that IL-6 levels were lower in those with depression. Similarly, for TNF-alpha, Meyer found 11 studies linking elevated TNF-alpha with depression, four with non-significant results, and none showing a negative relationship between TNF-alpha and depression. For c-reactive protein, six studies showed that c-reactive protein was elevated in people with depression, six had non-significant results, and none indicated that c-reactive protein was lower in depressed patients.
Most studies that have linked inflammation to depression have done so by measuring inflammatory markers in the blood. It is more difficult to measure inflammation in the brain of living people, but Meyer has taken advantage of new developments in positron emission tomography (PET) scans to measure translocator protein binding, which illustrates when microglia are activated. Microglial activation is a sign of inflammation. Translocator protein binding was elevated by about 30% in the prefrontal cortex, anterior cingulate cortex, and insula in study participants who showed symptoms of a major depressive episode compared to healthy control participants. The implication is that the depressed people with elevated translocator protein binding have more brain inflammation, probably via microglial activation.
The antibiotic minocycline reduces microglial activation. It would be interesting to see if minocycline might have antidepressant effects in people with depression symptoms and elevated translocator protein binding.
Inflammatory Markers of Bipolar Illness Course
 People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Ben Goldstein reported on a study that examined levels of TNF alpha, IL-6, and high sensitivity CRP (hsCRP) in 123 adolescents with an average age of 20.4 years, who had been ill for an average of 12.7 years.
CRP levels in adolescents with bipolar illness were equivalent to those with rheumatoid arthritis, and much higher than healthy controls. In children with bipolar disorder, higher levels of CRP were related to more time symptomatic. High hsCRP was related to lower socio-economic status and to substance abuse disorders.
Increases in IL-6 were linked to a longer time to achieve remission and more weeks depressed. High IL-6 was related to duration of illness, positive family history of substance use, and family conflict.
High TNF alpha was related to low socioeconomic status (SES), self-injury, suicidal ideation, and positive life events.
Goldstein said studies of these markers could eventually lead to therapeutic advances, but the process would be long and would require several steps: proof of concept studies, prospective validation studies in independent samples, and demonstration of clinical gains over standard predictive markers, culminating in enhanced patient care and outcome through better, faster prediction of response.
Editor’s Note: Ideally clinicians could jump ahead by immediately attempting to determine whether adding a medication with direct anti-inflammatory effects could enhance therapeutic effects in children with elevated inflammatory markers. Treating inflammation could also theoretically help prevent cognitive deterioration and decrease the considerable risk for cardiovascular dysfunction in patients with bipolar disorder.