Young Men at Highest Schizophrenia Risk From Cannabis Abuse
Roughly 15% of schizophrenia cases among young males may be preventable by avoiding cannabis use disorder (CUD). Not only does cannabis abuse markedly increase the risk of schizophrenia, its use has transgenerational effects such that offspring from a cannabis user are more prone to use opiates.
Editors Note: Youngsters need to know two things.
1. Any supposedly legitimate drug bought on line may look like the real thing, but it is all-too-often laced with fentanyl which can kill someone in 5 minutes. No street-bought drug is safe, no matter how real it looks.
2. Marijuana will not kill you, but can make you psychotic for the rest of your life. The widely circulated notion that pot is safe is just a conspiracy by the plant growers to make money and by politicians who are ignorant of the facts. Pot doubles the rate of paranoia in the general population and if you have a good functioning genetic (val158val) version of COMT, this works too well to deplete dopamine in the prefrontal cortex and further increases the risk of paranoia and psychosis.
Familial Aggregation of Major Depression Predicts Risk of Major Depression
Gronemann et al reported in JAMA Psychiatry: “In this cohort study of 2,903,430 individuals, maternal, paternal, full sibling, or half-sibling with MD were associated with 2-fold higher risks of MD in men and women….(E)xposure to family MD during childhood and adolescence was associated with increased risk. The risk increased with number of affected family members; (however) individuals exposed when 30 years or older had markedly lower risk.”
Editors Note: Even depression in grandparents adds further to the risk of depression. When there is high familial loading for depression and other psychiatric illnesses, one should be alert to the possible onset of depression in young individuals and treat them early and well accordingly.
Psychiatric Risks in Offspring of Parents with Bipolar/Unipolar Disorders
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Martin Preisig and colleagues from Lausanne, Switzerland reported on a longitudinal study of mood disorders in offspring of parents with bipolar disorder, unipolar depression, or no history of psychiatric illness. The study included 446 children (with an average age of 10.1 years at the beginning of the study), who participated for an average of 11.9 years.
Preisig and colleagues determined symptoms and other factors that preceded psychiatric illness. They found that bipolar disorder in the offspring was preceded by sub-threshold hypomania, major depression, and conduct disorder. Bipolar disorder in the offspring was also predicted by parental early-onset bipolar disorder.
Major depression was preceded by separation anxiety disorder, and witnessing violence or being a victim of sexual abuse.
Preisig and colleagues concluded that not only did bipolar disorder and major depressive disorder have different familial origins, they also had different antecedents and risk factors.
Early Predictors of Suicide and Lithium as an Anti-Suicide Drug
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
Editor’s Note: Among all psychotropic drugs, lithium has the best data supporting its anti-suicide effects, both at therapeutic doses in patients with bipolar disorder and at trace levels in the water supply in the general population. People who live in locations where more lithium is naturally present in the water supply have lower rates of suicide than those who live in places with less lithium in the water. Malhi also noted that the antioxidant N-acetylcysteine (NAC), which has positive effects on mood and habitual behaviors, can reduce the incidence of lithium-induced dysfunction of the kidneys.
In Danish Study, Higher Trace Levels of Lithium in Drinking Water in Certain Regions Do Not Seem to Prevent Bipolar Disorder
Previous studies have found that trace levels of lithium that occur naturally in the drinking water of certain regions are associated with lower rates suicide. Preliminary studies have also shown that lithium in drinking water is associated with lower dementia rates. The trace levels seen in drinking water are many hundreds of times lower than clinical doses of lithium prescribed for bipolar disorder, but they vary greatly according to locality.
A new study by researcher Lars Kessing and colleagues investigated whether chronic exposure to lithium in drinking water might protect against bipolar disorder, but found no evidence that this is the case in Denmark.
In an article published in the journal Bipolar Disorders in 2017, Kessing and colleagues describe findings from their analysis of data on 14,820 patients with a diagnosis of mania or bipolar disorder and (for each participant with bipolar disorder) 10 other age- and gender-matched control participants totaling 140,311. The researchers were able to look longitudinally at the participants’ exposure to trace levels of lithium in drinking water based on their municipalities of residence.
The investigators hoped to find evidence that greater exposure to lithium was associated with lower rates of bipolar disorder. Kessing and colleagues concluded that trace lithium levels higher than those in Denmark might be needed to find such a result.
Editor’s Note: Clinical studies of lithium treatment for children at high risk for bipolar disorder could help clarify whether even conventional therapeutic levels of lithium could reduce or delay the appearance of bipolar disorder.
Father’s Age, Behavior Linked to Birth Defects
For decades, researchers have known that a pregnant mother’s diet, hormone levels, and psychological state can affect her offspring’s development, altering organ structure, cellular response, and gene expression. It is now becoming clear that a father’s age and lifestyle at the time of conception can also shape health outcomes for his offspring.
Older fathers have offspring with more psychiatric disorders, possibly because of increased incidence of mutations in sperm.
A 2016 article by Joanna Kitlinska and colleagues in the American Journal of Stem Cells reviewed findings from human and animal studies about the links between fathers’ behaviors and their offspring’s development.
Father’s behavior can shape gene expression through a phenomenon described as epigenetics. Epigenetics refers to environmental influences on the way genes are transcribed. While a father’s behavior is not registered in his DNA sequences, it can influence the structure of his DNA or the way in which it is packaged.
Kitlinska suggests that these types of findings should eventually be organized into recommendations for prospective parents. More research is also needed into how maternal and paternal influences interact with each other.
Some findings from the article:
- A newborn can have fetal alcohol spectrum disorder even if the mother doesn’t drink. “Up to 75% of children with [the disorder] have biological fathers who are alcoholics,” says Kitlinska.
- Father’s alcohol use is linked to low birth weight, reduced brain size, and impaired cognition.
- Dad’s obesity is linked to enlarged fat cells, diabetes, obesity, and brain cancer in offspring.
- A limited diet in a father’s early life may reduce his children and grandchildren’s risk of death from cardiovascular causes.
- Dad’s advanced age is correlated with higher rates of schizophrenia, autism, and birth defects in his children.
- Psychosocial stress on dads can affect their children’s behavioral traits.
Inflammatory Markers of Bipolar Illness Course
 People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
People with bipolar disorder often show signs of inflammation. These could eventually help clarify diagnosis, illness activity, and treatment response, and predict illness progression. Previous studies have shown increases in c-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha) in adults with mood disorder. These high levels tend to improve with medications, are related to illness severity, and are also related to manic and mixed states.
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Ben Goldstein reported on a study that examined levels of TNF alpha, IL-6, and high sensitivity CRP (hsCRP) in 123 adolescents with an average age of 20.4 years, who had been ill for an average of 12.7 years.
CRP levels in adolescents with bipolar illness were equivalent to those with rheumatoid arthritis, and much higher than healthy controls. In children with bipolar disorder, higher levels of CRP were related to more time symptomatic. High hsCRP was related to lower socio-economic status and to substance abuse disorders.
Increases in IL-6 were linked to a longer time to achieve remission and more weeks depressed. High IL-6 was related to duration of illness, positive family history of substance use, and family conflict.
High TNF alpha was related to low socioeconomic status (SES), self-injury, suicidal ideation, and positive life events.
Goldstein said studies of these markers could eventually lead to therapeutic advances, but the process would be long and would require several steps: proof of concept studies, prospective validation studies in independent samples, and demonstration of clinical gains over standard predictive markers, culminating in enhanced patient care and outcome through better, faster prediction of response.
Editor’s Note: Ideally clinicians could jump ahead by immediately attempting to determine whether adding a medication with direct anti-inflammatory effects could enhance therapeutic effects in children with elevated inflammatory markers. Treating inflammation could also theoretically help prevent cognitive deterioration and decrease the considerable risk for cardiovascular dysfunction in patients with bipolar disorder.
Possible Interventions for At-Risk Children in Addition to Family Focused Therapy
Our editor Robert M. Post recommends that in the absence of good care in the community for children at high risk for bipolar disorder because a parent has the disorder, adult psychiatrists of parents with bipolar disorder who have children with the disorder should fill this gap by treating the children themselves. If the child has only early symptoms, family focused therapy as developed by David Miklowitz would be recommended.
Here are some other suggestions in addition to family focused therapy:
- Good Diet, Exercise, Sleep Hygiene
- Omega-3 Fatty Acids
- Check Vitamin D3 levels and Add Supplement if Needed
- Melatonin for Insomnia
- N-acetylcysteine (NAC) for Irritability (as in studies of children with autism spectrum disorders)
- Folate for Depression and/or Elevated Homocysteine
- Check for Evidence of Inflammation (Increased IL-6 or CRP)
Options with Some Side Effects:
- Minocycline (an anti-inflammatory neuroprotective antibiotic)
Heading Off Early Symptoms of Bipolar Disorder in Children at High Risk
 At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
At the American Academy of Child and Adolescent Psychiatry (AACAP) annual meeting in Toronto in October 2011, there was a symposium on risk and resilience factors in the onset of bipolar disorder in children who have a parent with the disorder.
Family Focused Therapy Highly Encouraged
Amy Garrett reported that family focused therapy (FFT) in those at risk for bipolar disorder was effective in ameliorating symptomatology compared to treatment as usual. Family focused therapy, pioneered by Dave Miklowitz, PhD of UCLA involves three components. The first component is education about the illness and methods of self-management. The second is enhancement of communication in the family with practice and rehearsal of new modes of conversation. The third component is assistance with problem solving.
In Garrett’s study, 50 children aged 7 to 17 were randomized to family focused treatment or treatment as usual. These children were not only at high risk for bipolar disorder, they were already prodromal, meaning they were already diagnosable with bipolar not otherwise specified (BP-NOS), cyclothymia, or major depressive disorder, and had also shown concurrent depressive and/or manic symptoms in the two weeks prior to the study. At baseline, compared to controls, these children at high risk for full-blown bipolar disorder by virtue of a parental history of the illness showed increased activation of the amygdala and decreased activation of the prefrontal cortex. Most interestingly, after improvement with the family focused therapy (FFT), amygdala reactivity to emotional faces became less prominent and dorsolateral prefrontal cortical activity increased in proportion to the degree of the patient’s improvement.
The discussant for the symposium was Kiki Chang of Stanford University, who indicated that the results of this study of family focused therapy were already sufficient to convince him that FFT was a useful therapeutic procedure in children at high risk for bipolar disorder by virtue of having a parent with a history of bipolar illness. Chang is now employing the therapy routinely in all of his high-risk patients.
Editors Note: This is an extremely important recommendation as it gives families a specific therapeutic process in which to engage children and others in the family when affective behavior begins to become abnormal, even if it does not meet full criteria for a bipolar I or bipolar II disorder.
FFT also meets all the important criteria needed for putting it into widespread clinical practice. Family focused therapy has repeatedly been shown to be effective in adults and adolescents with bipolar illness and now also in these children who are prodromal. The psychoeducational part of FFT is common sense, and dealing with communication difficulties and assisting with problem solving also have merit in terms of stress reduction. Finally, this treatment intervention appears to be not only safe but also highly effective in a variety of different prodromal presentations of affect disorders even if children do not meet full criteria for bipolar disorder. While the few studies of early intervention with psychopharmacological agents have not yet identified efficacious medications for the prodromes of bipolar disorder and in particular medications with a high degree of safety, such family focused therapy appears to be an ideal early intervention.
I would concur with Dr. Chang’s assessment. Family focused therapy (FFT) should be offered to all children with this high-risk status who have begun to be symptomatic. Early onset of unipolar depressive disorder or of bipolar disorder carries a more adverse prognosis than the adult onset variety and thus should not be ignored. If more serious illness is headed off early, it even raises the possibility that the full-blown illness will not develop at all.
Gray Matter Volume Abnormalities
Tomas Hajek of Dalhousie University in Halifax presented data indicating that in children at high risk for bipolar disorder, gray matter volume in the right inferior frontal gyrus is increased. Read more
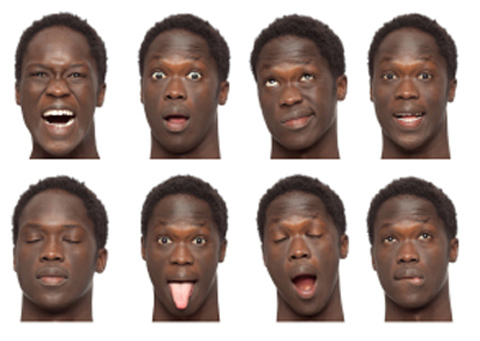
Consistent Deficits In Facial Emotion Recognition Found in Non-Ill Children of Parents with Bipolar Disorder
Children with bipolar parents may have difficulty identifying the emotions they see on another person’s face. Aditya Sharma of Newcastle University presented a poster at the Pediatric Bipolar Conference in Cambridge, Massachusetts in March, which indicated that children without bipolar disorder but at risk because a parent has the illness showed deficits in facial emotion recognition. Similar results were reported by Brotman et al. in the American Journal of Psychiatry in 2008. Since children of bipolar parents are at increased risk of developing the disease, this deficit in labeling facial emotion may be a marker of early bipolar disorder or a risk factor for its onset.
Editor’s Note: These types of deficits in facial emotion recognition have been consistently observed in adults and children diagnosed with bipolar disorder, so assessing whether children can successfully identify others’ facial emotions could become part of the assessment of risk for bipolar disorder. This deficit could also be targeted for psychosocial intervention and rehabilitative training to enhance emotion recognition skills. Such an approach could improve interpersonal communication and lessen hypersensitive responses to perceived emotional threats and negative emotional experiences.