Quetiapine is Effective Across a Spectrum of Illnesses
The atypical antipsychotic quetiapine (Seroquel or Seroquel XR) has a range of efficacy in a number of illnesses, depending on the size of the dose given. Read about some of its uses below, including as an adjunct to antidepressants in unipolar depression; as a treatment for generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD); and, at higher doses, as a treatment for mania and depression. Some of its potential mechanisms of action are described as well.
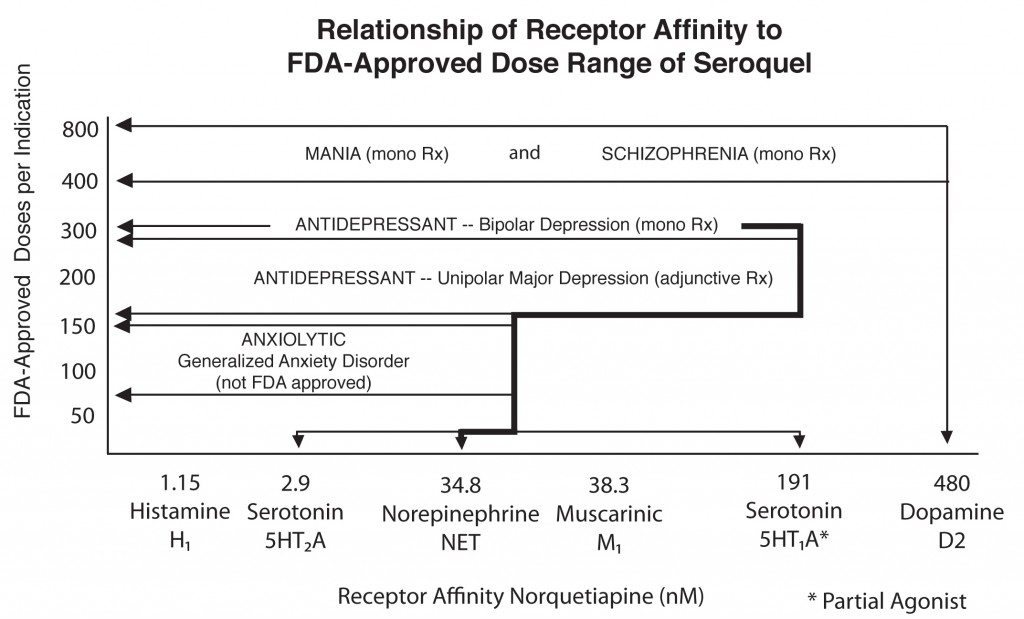
Quetiapine's actions on various receptors in the brain (bottom axis) are responsible for its effects in different illnesses
Quetiapine as an adjunct to antidepressants in unipolar depression
Posters at the American Psychiatric Association meeting in San Francisco in May 2009 showed new data from a series of studies of quetiapine in unipolar depression that showed the drug in monotherapy (at 150mg & 300mg) was significantly more effective than placebo. Studies were also positive when quetiapine was used as an adjunct compared with placebo for patients showing inadequate or incomplete responses to antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Quetiapine has previously been approved for monotherapy treatment of schizophrenia, acute mania, and acute bipolar depression, and is also approved to be used in combination with either lithium or valproate for prevention of both manic and depressive episodes.
Based on this new series of studies in unipolar (UP) depression, the FDA has approved quetiapine (Seroquel XR), but only as an adjunct to previously unsuccessful antidepressants for UP depression. The side effects demonstrated in these studies were similar to those previously reported in schizophrenia, mania, and bipolar depression. These included a moderate incidence of sedation and somnolence (sleepiness) with a 1kg to 2kg increase in weight in most of the studies. There was also a slightly increased risk for increases in some of the indices of the metabolic syndrome, including levels of fasting blood glucose, triglycerides, and the low-density lipoprotein component of cholesterol.
These studies were all performed with the extended release form of the drug (Seroquel XR), which it is recommended to administer three to four hours prior to bedtime. With the XR preparation, blood levels reach a peak of 400ng/ml five or six hours after the administration of a single evening-time dose. With the original immediate release preparation, much higher blood levels (800ng/ml) occurred in the first hour after a dose, so it was recommended that the original preparation be administered immediately prior to bedtime.
The XR preparation comes in 50mg capsules, and it is recommended that the dose be titrated with 50mg increases each day until the target of 150mg (nighttime dose) is achieved on the third day. However, in those with problematic degrees of somnolence and sedation carrying over to the next morning, it is advisable to slow down the titration until these side effects wane. Since a few percent of patients will have difficulty getting up early in the morning after a single nighttime dose, a test dose on a Friday or Saturday night has been recommended by Dr. Joseph Calabrese for those with important morning work or school schedules.
Quetiapine in Generalized Anxiety Disorders (GAD)
Another poster described the effects of Seroquel XR in generalized anxiety disorder. Its use was associated with significant degrees of improvement on most outcome measures compared with placebo, including improvements in anxiety, somatic symptoms, and sleep. Doses administered were 75mg and 150mg given at night. Despite these positive efficacy data, the FDA advisory panel had concerns about its tolerability, and decided not to approve quetiapine for treatment of GAD.
Quetiapine in post-traumatic stress disorder (PTSD)
In a poster about the use of quetiapine (Seroquel XR) in post-traumatic stress disorder (PTSD), doses of 150mg and 300mg were both more effective than placebo. The range of improvement included the entire PTSD syndrome measured by the Clinician-Administered PTSD Scale (CAPS), and in each of its subscales, including paroxysmal events (such as nightmares and flashbacks), generalized level of anxiety, numbing, and sleep disturbances (which are often particularly problematic in PTSD).
Different doses of quetiapine for different illnesses
As illustrated in the figure, there appears to be an interesting relationship between receptor affinity and FDA-approved dose range of seroquel across different psychiatric syndromes, suggesting that different doses are effective for different illnesses. The conventional dose for treating acute mania or schizophrenia is 400mg to 800mg/day. In contrast, lower doses in the range of 300mg to 600mg/day are indicated for acute treatment of bipolar depression; however, the 600mg/day dose is not significantly superior to 300mg/day. The adjunctive prophylactic efficacy of quetiapine compared with placebo in preventing manic and despressive episodes in bipolar disorder was established at 400mg/day added to ongoing treatment with either lithium or valproate. Doses of quetiapine adequate for unipolar depression, generalized anxiety disorder, and PTSD appear to reside in a lower range (150mg to 300mg/day).
Mechanisms of action of quetiapine potentially related to its effectiveness
The wide range of efficacy of quetiapine across a number of psychotic syndromes (schizophrenia and mania) and mood and anxiety disorders makes one wonder about the mechanisms by which the drug works. While none of quetiapine’s specific actions on different neurotransmitters has been definitively linked to efficacy in a given syndrome, a variety of hypotheses remain particularly appealing.
Weak blockade of dopamine receptors implicated in actions in mania and schizophrenia
The blockade of dopamine receptors has long been implicated in the mechanisms of antipsychotic and antimanic drugs, and this remains a likely mechanism for quetiapine’s effects. However, quetiapine has a low affinity in blocking dopamine D2 receptors, or a low degree of binding to those receptors, and its rapid dissociation from the receptor may be a reason that higher doses are needed for mania and schizophrenia. Even at these higher doses, it rarely causes acute Parkinsonian effects or increases plasma prolactin, which are both direct effects of potent D2 receptor blockade.
New brain imaging data in humans also indicate that quetiapine (like clozapine, the most effective atypical antipsychotic that also features the least motor side effects) binds less tightly to dopamine receptors in the motor areas of brain (striatum) than in extrastriatal areas, which could also explain its relative lack of Parkinsonian side effects.
Potential antidepressant mechanisms
Quetiapine’s ability to block 5HT2 receptors is shared by most atypical antipsychotics and is thought to contribute to their benign motor side-effects profile. Such a blockade has also been implicated in antidepressant effectiveness and in enhancing slow wave sleep not only with the atypicals, but also with antidepressants such as trazodone and nefazodone.
Quetiapine’s active metabolite norquetiapine has extra actions not shared by the parent compound. Norquetiapine blocks the norepinephrine transporter, with potencies in a range similar to that of traditional noradrenergic-selective antidepressants such as desipramine, nortriptyline, and malprotiline. This action could account for some of quetiapine’s antidepressant and anti-anxiety efficacy. In addition, norquetiapine is a 5HT1A partial agonist and thus shares some of the effects of the more selective serotonin 5HT1A agonist buspirone (Buspar), which exhibits some antidepressant and antianxiety effects.
Norquetiapine also blocks 5HT2C receptors, which inhibit release of norepinephrine and dopamine into the prefrontal cortex. Since norquetiapine is an antagonist of these receptors, it increases dopamine and norepinephrine release in the prefrontal cortex via disinhibition (an action shared by ziprasidone (Geodon). Hypofunction of prefrontal cortex has been implicated in many primary and secondary depressive syndromes, so it remains plausible that norquetiapine’s action at the 5HT2C receptors could be implicated in its antidepressant efficacy.
In animal studies, quetiapine increases levels of brain-derived neurotrophic factor (BDNF) in the hippocampus and prevents stress from decreasing BDNF. BDNF is necessary for long-term learning and memory as well as neural and glial health and survival. BDNF in patients’ blood decreases with depressive episodes in proportion to their severity, and all known antidepressants appear to increase BDNF. Thus, effects on BDNF may also explain some of quetiapine’s antidepressant actions.
Potential mechanisms related to side effects
Quetiapine also potently blocks histamine (H1) and muscarinic acetylcholinergic receptors (M1), actions that could account for some of its side-effects profile, including sedation (via H1 blockade), dry mouth and constipation (via M1 blockade). Recent data indicate that intravenous doses of the selective blocker of muscarinic receptors scopolamine cause rapid antidepressant effects, so it is possible that quetiapine’s ability to block M1 could also contribute to its antidepressant effects. Quetiapine also blocks noradrenergic ?1 receptors, which could explain orthostatic hypertension (low blood pressure upon standing), an occasional side effect.
Overview: Dose requirements correlate with receptor affinities
Quetiapine’s blockade of the D2 receptor is weak. To the extent that D2 receptor blockade is implicated in antimanic and antipsychotic effects, higher doses of quetiapine are required to maximally exert this action. In contrast, the greater potency of norquetiapine for blockade of the norepinephrine reuptake transporter is in line with the lower doses required to treat depression.
The high potency of quetiapine in blocking histamine and cholinergic receptors would also be compatible with the high to moderate sedative and anticholinergic effects of the drug as well. For some patients, these side effects can be problematic even at the lowest doses.
Comments
One Response to “Quetiapine is Effective Across a Spectrum of Illnesses”
Leave a Reply


is there a maximum dose you can use for a 13 years with autism for irritability and the behavior is not controlled with 700mg daily.