30 Minutes of TDCS Better Than 20 Minutes in Patients with Unipolar Depression
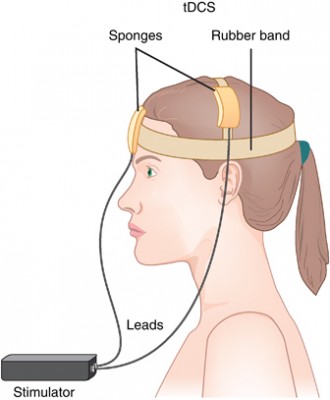 Transcranial direct current stimulation (tDCS) has successfully been used to treat depression. In this treatment, electrodes applied to the scalp provide a constant low level of electricity that can modulate neuron activity. In a 2017 article in the journal Progress in Neuro-Psychopharmacology & Biological Psychiatry, researcher Elena L. Pavlova and colleagues report that both 20- and 30-minute sessions of tDCS improved mild to moderate depression when combined with the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline. However, the 30-minute sessions produced more improvement in depression.
Transcranial direct current stimulation (tDCS) has successfully been used to treat depression. In this treatment, electrodes applied to the scalp provide a constant low level of electricity that can modulate neuron activity. In a 2017 article in the journal Progress in Neuro-Psychopharmacology & Biological Psychiatry, researcher Elena L. Pavlova and colleagues report that both 20- and 30-minute sessions of tDCS improved mild to moderate depression when combined with the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline. However, the 30-minute sessions produced more improvement in depression.
In the study, 69 right-handed patients (average age 37.6) received 50 mg of sertraline (Zoloft) per day and were randomized to one of three tDCS conditions: 10 daily 30-minute sessions, 10 daily 20-minute sessions, or 10 daily sham sessions with no tDCS treatment. The tDCS consisted of 0.5mA anodal current to the left dorsolateral prefrontal cortex.
Both 30-minute and 20-minute tDCS sessions produced greater benefit than the sham sessions. The 30-minute group showed significantly greater percentage improvement in depression scores than the 20-minute group, and included more participants who responded to treatment (89% compared to 68% of the 20-minute group and 50% of the sham group) and more whose depression remitted (70% compared to 27% of the 20-minute group and 35% of the sham group).
Combo of Memantine and Sertraline Effective for Unipolar Depression
A 2016 study in the Journal of Clinical Pharmacy and Therapeutics finds that the combination of memantine (Namenda), a drug used to treat Alzheimer’s disease, and the antidepressant sertraline (Zoloft) improved unipolar depression more than sertraline plus placebo.
The study by Meysam Amidfar and colleagues included 66 patients with moderate to severe unipolar depression. They were divided into two groups—one received sertraline plus memantine for six weeks, while the other received sertraline and a placebo.
The memantine group showed significantly greater improvement at 2 weeks, 4 weeks, and 6 weeks, and significantly greater response at 4 and 6 weeks. There were also more early improvers in the mematine group, and more rapid response to treatment. Both groups improved significantly over the six weeks of treatment.
Larger studies are needed to learn more about the safety and efficacy of memantine combined with sertraline for the treatment of unipolar depression, but this initial study is promising. In 2012, researcher Amit Anand and colleagues reported that in bipolar depression, memantine potentiates the effects of lamotrigine. Memantine also helped rapid cyclers when added to ongoing treatment in an open study of the drug treatment by Athanasios Koukopoulus and colleagues in 2012.
Combination of SSRIs and Statins Better than SSRIs Alone
A large study in Denmark suggests that taking selective serotonin reuptake inhibitor (SSRI) antidepressants alongside cholesterol-lowering statin drugs improved depression more than SSRIs alone. The findings, by Ole Köhler and colleagues were reported in the American Journal of Psychiatry in 2016.
The study included 872,216 people in Denmark’s national health care database who took SSRIs between 1997 and 2012. The most common SSRIs were citalopram, sertraline, and escitalopram. Of these people taking SSRIs, 13.0% also took a statin drug, typically simvastatin. Those patients who were taking both an SSRI and a statin were less likely than those taking an SSRI alone to be hospitalized for any psychiatric problem, or for depression specifically.
Depression is known to be correlated with inflammation throughout the body. Statins reduce this inflammation as well as lowering cholesterol. A 2013 study by Ahmad Ghanizadeh and Arvin Hedayati in the journal Depression and Anxiety showed that the SSRI fluoxetine and the statin lovastatin reduced depression severity compared to fluoxetine alone.
The combination of SSRIs and statins did not seem to reduce deaths or suicidal behavior compared to SSRIs alone. Statins have some side effects, but combining them with antidepressants did not increase the risks associated with their use.
Weight Gain is a Common Issue with Antidepressants, But Buproprion is an Exception
A 2016 study by researcher David Arterburn and colleagues in the Journal of Clinical Medicine suggests that taking an antidepressant for two years is associated with an increase in body weight. Luckily, bupropion (trade name Wellbutrin) is an exception that may be a good choice for obese or overweight patients.
The researchers analyzed links between which antidepressants patients in a large health system in Washington State were prescribed and their body weight two years later.
The researchers used fluoxetine (Prozac) as a reference. Most antidepressants did not differ significantly from fluoxetine in terms of the weight gain experienced by people taking the drug.
There were a few exceptions. Compared to non-smoking fluoxetine users, who gained an average of 4.6 pounds in two years, non-smoking bupropion users actually lost weight—an average of 2.4 pounds. (Smokers taking bupropion still gained an average of 6.9 pounds.)
Sertraline (Zoloft) was another exception. Sertraline users gained more than users of other antidepressants—an average of 10.5 pounds over two years.
Most SSRIs Free of Birth Defect Risk Early in Pregnancy, Fluoxetine and Paroxetine are Exceptions
A large study of women who took selective serotonin reuptake inhibitor (SSRI) antidepressants in the month before pregnancy and throughout the first trimester suggests that there is a smaller risk of birth defects associated with SSRI use than previously thought, though some risks were elevated in women who took paroxetine or fluoxetine.
The 2015 study, by Jennita Reefhuis and colleagues in the journal BMJ, investigated the drugs citalopram, escitalopram, fluoxetine, paroxetine, and sertraline, and examined birth defects that had previously been associated with SSRI use in smaller studies. The participants were 17,952 mothers of infants with birth defects and 9,857 mothers of infants without birth defects who had delivered between 1997 and 2009.
Sertraline was the most commonly used SSRI among the women in the study. None of the birth defects included in the study were associated with sertraline use early in pregnancy. The study found that some birth defects were 2 to 3.5 times more likely to occur in women who had taken fluoxetine or paroxetine early in their pregnancies.
Five different birth defects, while uncommon, were statistically linked to paroxetine use: anencephaly (undersized brain), heart problems including atrial septal defects and right ventricular outflow tract obstruction defects, and defects in the abdominal wall including gastroschisis and omphalocele. Two types of birth defects were associated with fluoxetine use: right ventricular outflow tract obstruction defects and craniosynostosis (premature fusion of the skull bones). Absolute incidence of these defects was also low.
Transcranial Direct Current Stimulation Plus Zoloft Has Better Antidepressant Effects Than Either Treatment Alone
 Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
The six-week study used what is called a 2×2 factorial design, in which 120 patients with unipolar depression received either 50 mg/day of sertraline or placebo and also received either real tDCS or a sham procedure. The tDCS was administered in twelve 30-minute sessions, one per day Monday through Friday during the first two weeks, followed by one every other week. TDCS consists of an anodal (positive) and cathodal (negative) current placed at particular positions on the head. This study used 2 microamps of anodal left/cathodal right prefrontal stimulation for the tDCS treatment.
While the combination of sertraline and tDCS was significantly better than all three other treatment options (sertraline plus sham procedure, placebo plus tDCS, and placebo plus sham procedure), sertraline by itself and tDCS by itself resulted in similar efficacies. However, TDCS by itself was also significantly better than placebo, while sertraline by itself was not.
Side effects among the different treatment options were similar, except those who received tDCS had more scalp redness. There were seven instances of patients developing mania or hypomania during the study, five of which occurred in the combined tDCS and sertraline treatment group, higher than the 1–2% rate that would be expected in a study of unipolar depression.





