Baseline Levels of CRP Could Help Predict Clinical Response to Different Treatments
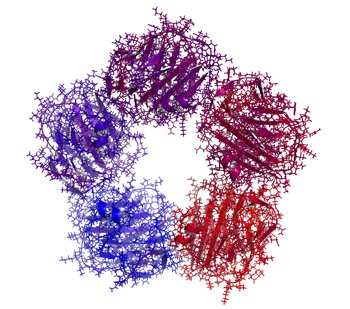
C-reactive protein, or CRP, is a marker or inflammation that has been linked to depression and other illnesses. People with high levels of CRP respond differently to medications than people with lower CRP, so assessing CRP levels may help determine which medications are best to treat a given patient.
High baseline levels of CRP (3–5pg/ml) predict a poor response to selective serotonin reuptake inhibitor antidepressants (SSRIs) and to psychotherapy, and are associated with increased risk of recurrent depression, heart attack, and stroke.
However, high baseline CRP predicts a better response to the antidepressants nortriptyline and bupropion. High CRP is also associated with better antidepressant response to infliximab (a monoclonal antibody that inhibits the inflammatory cytokine TNF alpha), while low levels of CRP predict worsening depression upon taking infliximab.
High baseline CRP also predicts good antidepressant response to intravenous ketamine (which works rapidly to improve treatment-resistant depression), minocycline (an anti-inflammatory antibiotic that decreases microglial activation), L-methylfolate (a supplement that can treat folate deficiency), N-acetylcysteine (an antioxidant that can improve depression, pathological habits, and addictions), and omega-3 fatty acids (except in people with low levels of DHA).
High baseline CRP also predicts a good response to the antipsychotic drug lurasidone (marketed under the trade name Latuda) in bipolar depression. In people with high baseline CRP, lurasidone’s positive results have a huge effect size of 0.85, while in people with low CRP (<3pg/ml) the improvement on lurasidone has a smaller effect size (0.35).
In personal communications with this editor (Robert M. Post) in 2018, experts in the field (Charles L. Raison and Vladimir Maletic) agreed that assessing baseline CRP levels in a given patient could help determine optimal strategies to treat their depression and predict the patient’s responsiveness to different treatment approaches.
At a 2018 scientific meeting, researchers Cynthia Shannon, Thomas Weickert, and colleagues reported that high baseline levels of CRP were associated with symptom improvement in patients with schizophrenia when they were treated with the drug canakinumab (marketed under the trade name Ilaris). Canakinumab is a human monoclonal antibody that targets the inflammatory cytokine interleukin-1 beta (Il-1b). Il-1b is elevated in a subgroup of patients with depression, bipolar disorder, or schizophrenia, and CRP levels are an indication of the associated inflammation.
Systematic Review Finds Bupropion is Effective for ADHD in Young People
 A 2016 systematic review by Qin Xiang Ng in the Journal of Child and Adolescent Psychopharmacology found that the antidepressant bupropion (Wellbutrin) can improve attention deficit hyperactivity disorder (ADHD) in children and adolescents.
A 2016 systematic review by Qin Xiang Ng in the Journal of Child and Adolescent Psychopharmacology found that the antidepressant bupropion (Wellbutrin) can improve attention deficit hyperactivity disorder (ADHD) in children and adolescents.
The review identified 25,455 studies of bupropion for ADHD, but only six included children. All six studies showed that bupropion improved ADHD symptoms in children and adolescents. Head-to-head trials of bupropion and methylphenidate (one of the most common medications to treat ADHD, which most people know by the name Ritalin) found the drugs had similar efficacy rates, although a large double-blind, placebo-controlled multicenter study found that bupropion had a smaller effect size than methylphenidate.
In terms of side effects, methylphenidate was more likely to cause headaches than bupropion, but otherwise the drugs were similar.
Ng suggests that bupropion should be considered for the treatment of ADHD in children and adolescents, but more large trials of the drug are needed. Bupropion may also help children whose ADHD appears alongside conduct, substance abuse, or depressive disorders.
Weight Gain is a Common Issue with Antidepressants, But Buproprion is an Exception
A 2016 study by researcher David Arterburn and colleagues in the Journal of Clinical Medicine suggests that taking an antidepressant for two years is associated with an increase in body weight. Luckily, bupropion (trade name Wellbutrin) is an exception that may be a good choice for obese or overweight patients.
The researchers analyzed links between which antidepressants patients in a large health system in Washington State were prescribed and their body weight two years later.
The researchers used fluoxetine (Prozac) as a reference. Most antidepressants did not differ significantly from fluoxetine in terms of the weight gain experienced by people taking the drug.
There were a few exceptions. Compared to non-smoking fluoxetine users, who gained an average of 4.6 pounds in two years, non-smoking bupropion users actually lost weight—an average of 2.4 pounds. (Smokers taking bupropion still gained an average of 6.9 pounds.)
Sertraline (Zoloft) was another exception. Sertraline users gained more than users of other antidepressants—an average of 10.5 pounds over two years.
Bupropion Plus Naltrexone Reduces Brain Response to Food Cues
The combination of antidepressant bupropion (Wellbutrin) and naltrexone (Revia), a drug that helps alcoholics resist the craving for alcohol, can help patients keep their weight down. Last year we summarized an article by Smith et al. in the journal Diabetes, Obesity, and Metabolism that showed that obese patients with diabetes treated with the combination of bupropion and naltrexone had excellent weight loss and reduction in body fat compared to those treated with either drug alone or with placebo.
A more recent study by G. J. Wang et al. published in the International Journal of Obesity in 2013 shows that the combination of 360mg of bupropion sustained release and 32mg of naltrexone sustained release works by reducing patients’ response to food cues. Forty women were shown a video of their favorite food being prepared, which stimulated parts of the brain associated with visual stimuli and other functions. Those who received the combination of naltrexone and bupropion had lessened hypothalamic response to the videos compared to those who received placebo, and also showed activity in parts of the brain associated with inhibitory control (the anterior cingulate), internal awareness (the superior frontal cortex, the insula, and the superior parietal cortex), and memory (the hippocampus).
Editor’s Note: It looks like the drug combination prompts the brain to say, “Wow, that looks good, but maybe I shouldn’t take in any more calories today.”