Ultrabrief Right Unilateral ECT Similar in Efficacy to Brief ECT with Fewer Side Effects
 A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
Loo and colleagues analyzed the findings of six different studies that compared right unilateral standard brief pulse ECT with ultrabrief pulse ECT and included a total of 689 patients. Standard ECT was more effective, producing more improvement in mood and more remissions, and working faster than ultrabrief ECT. However, standard ECT also produced greater cognitive side effects in every area tested, including thinking, learning and recall, and memory.
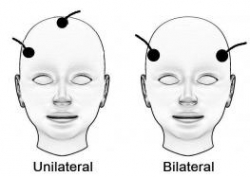
(When bilateral ECT is used, the cognitive effects are even worse, and researcher Harold Sacheim and colleagues have reported that the severity of the impairment in autobiographic memory is directly proportional to the number of bilateral ECT treatments a patient received, even when measured one year after the last session of bilateral ECT. This editor (Robert Post) believes bilateral ECT should be avoided if at all possible, as cognitive side effects can occasionally be severe.)
When Loo and colleagues removed nonrandomized trials from the analysis, the differences in efficacy between ultrabrief and standard right unilateral ECT were not statistically significant. Loo told Medscape Medical News that while the differences in efficacy between brief and ultrabrief ECT are minimal, the differences in side effects are greater. Right unilateral ultrabrief ECT works about as well as standard right unilateral brief pulse ECT, but preserves patients’ cognitive function better.
RTMS in the Elderly and After ECT
At the 2015 meeting of the Society of Biological Psychiatry in May, researcher Daniel Blumberger reported to this editor (Robert M. Post) that he has found repeated transcranial magnetic stimulation (rTMS) to be effective for depression in late life. Blumberger noted that it may be necessary to use higher intensity stimulation (i.e. at 120% of motor threshold instead of the usual 110% of motor threshold) in the elderly in order to overcome the gap between the skull and the brain, which can grow with age due to brain atrophy.
Blumberger has also successfully used rTMS as a followup treatment to a successful course of electroconvulsive therapy (ECT), administering rTMS twice a week for up to 66 treatments in a given patient in order to maintain remission of their depression.
RTMS Parameters
 As we wrote yesterday, repeated transcranial magnetic stimulation (rTMS) is a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain. The major studies of rTMS, by O’Reardon and colleagues (2007) and George et al. (2010), were performed with patients who were medication-free during the course of rTMS treatment. However, it is routine clinical practice to use rTMS as an adjunctive treatment to ongoing antidepressant therapy, and in these cases, response rates appear to be close to 50%, even in patients with considerable treatment resistance to prior antidepressants.
As we wrote yesterday, repeated transcranial magnetic stimulation (rTMS) is a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain. The major studies of rTMS, by O’Reardon and colleagues (2007) and George et al. (2010), were performed with patients who were medication-free during the course of rTMS treatment. However, it is routine clinical practice to use rTMS as an adjunctive treatment to ongoing antidepressant therapy, and in these cases, response rates appear to be close to 50%, even in patients with considerable treatment resistance to prior antidepressants.
Using the FDA-approved parameters, treatment is typically delivered with with an rTMS machine that stimulates the left prefrontal cortical area of the brain at a stimulation intensity of 120% of the patient’s motor threshold at a frequency of magnetic impulses of 10 per second or 10 Hz. The motor threshold is the intensity of stimulation necessary to cause the thumb to move when the motor cortex is stimulated, but the treatment is given over the frontal cortex which does not produce any movements or other sensations.
Each treatment lasts for about 20 minutes and does not require any anesthesia or premedication. The patient is awake and alert during the procedure, and cognitive side effects are minimal. Patients occasionally experience some pain from contraction of the scalp muscles under the magnet.
The rapid reversal of the magnetic field occurring ten times per second induces electrical stimulation of the brain at the same frequency and causes discharge of neurons. High frequency (at 10 or 20Hz) neuronal activity appears to increase activity (blood flow or metabolism) in the brain, while lower frequency stimulation, such as at 1 Hz, appears to decrease brain activity. In both cases, the effects last at least 48 hours after the last of a two- or three-week series of treatments. RTMS increases brain-derived neurotrophic factor (BDNF) in the brain, and BDNF is released when nerves fire at a fast frequency. The release of BDNF appears to be necessary for long-term learning and memory.
Sitting passively versus receiving therapy during rTMS
In clinical practice, most treatments are administered by a technician. However, in some instances, clinicians engage patients in forms of active psychotherapy while they are receiving the rTMS. Read more


