Obesity Linked to Illness Severity
In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher David Bond reported that 75% of patients in a study of first episode mania had unhealthy body mass indices (BMIs). Forty percent were overweight while thirty-five percent were obese. Higher weight was associated with greater illness severity. Bond said that in other studies obesity has been associated with less time well and a greater risk of relapse into depression.
Obese patients also had lower brain volume, worse memory, and a greater risk of developing early onset dementia compared to other patients. Those who were overweight or obese had a 35% higher risk of developing Alzheimer’s disease.
In a different talk at the same meeting, researcher Roger McIntyre reported that among patients with bipolar disorder, those who were obese have greater cognitive problems and more evidence of inflammation than those who were not obese. He has seen indirect antidepressant effects and other health benefits following weight loss from bariatric surgery.
Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
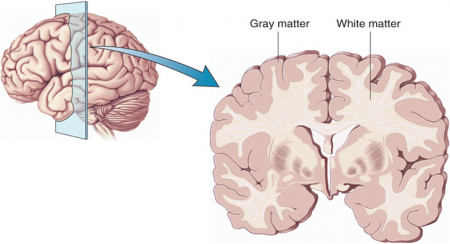
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.” Read more
Longitudinal Trajectory of Childhood Bipolar Disorder
Most children recover from an episode of bipolar disorder after a considerable period of time, but the majority eventually relapse. At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Boris Birmaher of the University of Pittsburgh presented new data on the long-term prospective course of bipolar disorder in 255 children with bipolar I, 30 children with bipolar II, and 153 children with bipolar NOS (not otherwise specified), who together had an average age of onset of 9.3 +/- 3.9 years. The children participated in the study for an average of 8 years. Most of the children (81.5%) recovered from their episode, but only after an average of 2.5 years of follow up treatment. Yet 62.5% of those who recovered experience a recurrence after an average of 1.5 years.
Editor’s Note: It takes a long, long time to achieve recovery, and longer for bipolar NOS (more than 2 years on average) than for either Bipolar I or II (about 1.8 years). However, the high rate of relapse within 1 to 2 years is equally disturbing. These data are similar to those in many other prospective follow up studies of children, and suggest that it is important for parents to be aware that this illness is difficult to treat, and good results within weeks are not likely to be the norm. At the same time, 43% of the children with a bipolar diagnosis eventually achieved euthymia (wellness) in the longer term, so there is cause for some optimism.
Four Trajectories in Children with Bipolar Illness
Birmaher described four different long-term,trajectories observed over an average of 8 years of follow up with 438 children with bipolar disorder.
- Predominately euthymic (24%)
- Ill early then much improved (19%)
- Mild to moderately ill—euthymic only 47% of the time (34.6%)
- Predominantly ill—euthymic 11.5% of the time (20.3%)
Explaining Wellness
The predominantly well group (1) was associated in a univariate analysis with a later onset of illness, higher socio-economic status, less conflict, fewer stressors, less sexual abuse, fewer anxiety and ADHD comorbidities, and less medication (including stimulant use). In a multivariate analysis, this group was independently associated with less severe depression/mania, less suicidal ideation, less substance use, less sexual abuse, and less family history of mania and substance abuse.
This group had the best functioning, almost to 80 on the Children’s Global Assessment Scale (C-GAS). In comparison, despite considerable time euthymic for groups 2 and 3, these children still had considerable functional impairment, in the realm of 65 on the C-GAS scale. Even in Group 1, about half of the children had low C-GAS scores.
Birmaher suggested the importance of trying to find ways to delay the onset of the illness (to graduate more children into the good prognosis group) and allowing them time to develop socially and educationally and graduate from high school. Potential preventive strategies could include omega-3 fatty acids, more time spent exercising, good sleep hygiene, family focused therapy (FFT), dialectic behavior therapy, treating subsyndromal depression, and even treating parents with mood disorders to complete remission (which has been shown to improve behavioral health in offspring).
Editor’s Note: As this editor Post, Chang, and Frye wrote in the Journal of Clinical Psychiatry in 2013, beginning to study the effectiveness of these kinds of early primary and secondary prevention strategies in children who can now be readily identified clinically as at risk for a mood disorder, should be given the highest priority.
Children who have at least one parent with a bipolar or unipolar disorder, some further environmental risk factors (such as adversity in early childhood), and early symptoms of depression, anxiety, or prodromal bipolar disorder are at very high risk for bipolar disorder, and there is an urgent need for randomized studies (even open ones) of safe potential preventive strategies for these children.
Omega-3 fatty acids in particular have a strong record of safety, compelling rationale for use in bipolar disorder, and have already been shown to have significant preventive effects in decreasing the transition from early prodromal psychosis to full-blown schizophrenia.