Inflammation and Depression: Treatment Implications
 Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Vladimir Maletic of the University of South Carolina School of Medicine Greenville gave a plenary talk at the 2018 meeting of the North Carolina Psychiatric Association that described a variety of ways that inflammation can drive depression.
Maletic explained that stress can increase neurotransmitters that activate brain macrophages, increase NFkB (a protein that controls DNA transcription and cell survival), and increase brain inflammation, evidenced by elevated levels of the inflammatory markers IL-1b, IL-6, TNF-alpha, and C-reactive protein (CRP). These signs of inflammation are associated with changes in brain function and connectivity that are consistent with depression, fatigue, and cognitive slowing.
Inflammation measured outside of the brain and spinal cord is associated with increased activity of the insula (a key brain sensor and modulator of emotions), disconnection between the prefrontal cortex and the reward circuits in the nucleus accumbens, and decreased function and structural changes to the hippocampus (critical for memory).
Maletic also explained that inflammation changes the way the amino acid tryptophan is metabolized. Normally tryptophan is converted into kyneurenic acid, which prevents excitotoxicity and has anticonvulsant effects. Stress can lead to tryptophan being metabolized instead into quinolinic acid, which is neurotoxic and has been linked to certain psychiatric disorders and neurodegenerative processes. This in turn impairs synaptic functioning, including increasing glutamate and decreasing brain-derived neurotrophic factor (BDNF), impairing a type of glia called oligodendroglia (which produce myelin), and the formation of new neural connections.
These findings have several important implications for treatment. Increases in inflammation have been linked to the atypical type of depression characterized by increased appetite, weight gain, and increased sleep rather than the more classic presentation of depression that includes loss of appetite, weight loss and insomnia. Thus, weight gain, waist circumference, and body mass index (BMI) are correlated with inflammation and can signal a poor response to medications (including the rapid-acting antidepressant ketamine and some other antidepressants). If someone with unipolar depression has high levels of CRP, they tend to have a poorer response to selective serotonin reuptake inhibitor (SSRI) antidepressants, and may respond better to the noradrenergic tricyclic antidepressant nortryptyline, the serotonin and norepinephrine reuptake inhibitors (SNRIs), and the dopamine active antidepressant bupropion.
There is some good news. Read more
Substance Abuse Is a Treatable Brain Disorder
Depression and bipolar disorder come with a high incidence of substance abuse. It is important to realize that there are now good medicines to treat the addictions as well as the primary mood disorders they accompany. At the 2015 meeting of the American Psychiatric Association, Nora Volkow, director of the National Institute of Drug Abuse, encouraged psychiatrists to think of addiction as a “disease of the brain that disrupts the systems that allow people to exert self-control,” saying that this would help reduce stigma both for insurance companies and for the wider public.
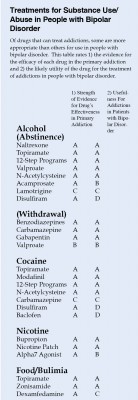
Most treatment of substance abuse in bipolar disorder is off-label. Doctors must infer indirect evidence of the possible efficacy of each drug in bipolar disorder from studies in those with only the primary addiction, for example, cocaine abuse without bipolar disorder.
The table at right is a preliminary rating of 1) the strength of the evidence for the efficacy of each drug in the primary addiction and 2) the likely utility of the drug for the treatment of addictions in people with bipolar disorder. For example, the drug baclofen has excellent evidence of efficacy in cocaine addiction, but gets a D for utility in bipolar disorder because baclofen can exacerbate depression.
This list is provisional, and the subjective grades for each drug are likely to change as more research is collected on these treatments. Consult a doctor if you are seeking treatment for bipolar disorder and/or substance abuse.
Effect Size of Autism Treatments
At the 2014 meeting of the American Academy of Child and Adolescent Psychiatry, Fung et al. presented a meta-analysis of treatments for autism that ranked them in terms of statistical effect size, ranging from 0.9 (large), to 0.5 to 0.8 (medium), to <0.4 (small). The only drug with a large effect size was risperidone, at 0.9. Most effect sizes were medium, including aripiprazole at 0.8 and N-acetylcysteine (NAC) at 0.7. Both clonidine and methylphenidate had effect sizes of 0.6, and tianeptine’s was 0.5.
Fung and colleagues noted that the first two on the list, the atypical antipsychotics risperidone and aripiprazole, often have problematic side effects (such as sedation, weight gain, and motor symptoms) that must be balanced against their effectiveness. In contrast, NAC is well tolerated with few side effects, and two placebo controlled studies showed that it was effective both alone and as an adjunctive treatment to the antipsychotic risperidone.