Accelerated iTBS Treats Bipolar Depression in 5 Days
Yvette Sheline, of the University of Pennsylvania Perelman School of Medicine, reported that 10 intermittent theta burst stimulations (iTBS) per day for 5 days yielded dramatic improvement in patients with bipolar depression – both immediately after the iTBS as well as at 4 weeks.
Resting-state functional MRI was used to individually target the left dorsolateral prefrontal cortex (dlPFC), the region most anticorrelated with the subgenual anterior cingulate cortex (sgACC).
Intermittent theta burst magnetic stimulation (iTBS) is FDA approved.
As reported in Psych. News:?The Food and Drug Administration (FDA) has cleared the SAINT Neuromodulation System for the treatment of refractory depression in adults, Magnus Medical Inc. (the manufacturer of the product)?announced?Tuesday. SAINT is a?modified form of transcranial magnetic stimulation?(TMS) that compresses weeks of conventional TMS therapy into just five days”. ?Regular TMS takes 20-30 minutes per daily session while iTBS takes about 5 minutes and thus can be applied many times in a single day. ?”As demonstrated in a clinical trial?published?in?The American Journal of Psychiatry, Montgomery-Åsberg Depression Rating Scale (MADRS) scores dropped by 62% among participants following five days of SAINT stimulation compared with a 14% drop among participants receiving sham stimulation. These improvements were sustained over a four-week follow-up.” ?The method was developed by Nolan Williams and he used MRI to best target the site of stimulation
Better One-Year Clinical Outcomes After Four Weeks of Theta Burst Stimulation for PTSD Than After Two Weeks

In a 2019 article in the journal Neuropsychopharmacology, Nicholas J. Petrosino and colleagues described findings from one year of follow-up with veterans suffering from post-traumatic stress disorder (PTSD) who received intermittent theta burst transcranial magnetic stimulation (iTBS) in a four-week crossover study.
In the first two weeks of the study, half of the 50 participants (who were mostly male and had an average age of 51) received iTBS while the others were given a sham procedure. Then all the participants received iTBS on an open (non-blind) basis for two more weeks.
At one month, those who had received four total weeks of iTBS had better outcomes than those who had received only two weeks of active iTBS. These results were published in the American Journal of Psychiatry in 2019 in an article by Noah S. Philip and colleagues.
The researchers went on to look at longer-term outcomes, namely time until relapse (a major event such as a re-hospitalization or suicide). After one year, those who received four weeks of iTBS went 9 to 11 months without relapsing (296.0 days ± 22.1), while those who received only two weeks of iTBS went 5 to 7 months before relapsing (182.0 days ± 31.9).
It seems that more iTBS may be better than less iTBS for PTSD in both the short and long term.
Three-Minute ‘Theta Burst’ Treatment as Effective as 37-Minute RTMS
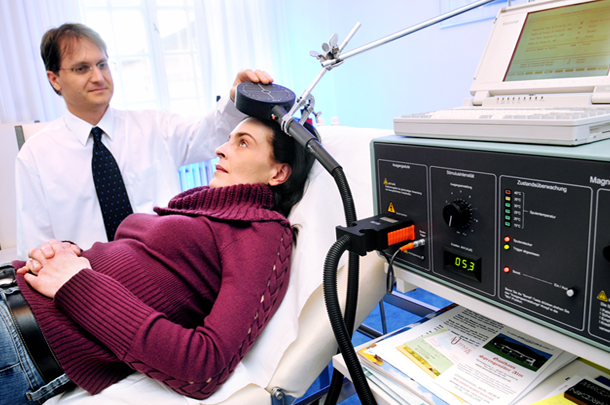
A variation on repeated transcranial magnetic stimulation (rTMS) called intermittent theta burst stimulation (iTBS) may be able to deliver the same benefits in a tenth of the time. RTMS is a non-invasive treatment in which a magnetic coil placed near the skull transmits electrical signals to the brain. It is effective in depression and has been shown to improve aspects of schizophrenia, autism, and addictions as well.
A typical rTMS session lasts for 37.5 minutes and consists of high frequency (10 Hz) stimulation. Access to the treatment remains somewhat limited, so the newer form of iTBS treatment may help more people access treatment by allowing clinicians to treat more patients in a day.
The 2018 study, published by Daniel Blumberger and colleagues in the journal The Lancet, compared iTBS to standard rTMS and evaluated the effectiveness, safety, and tolerability of the new treatment compared to the old. 414 patients aged 18–65 with major depression that had persisted despite treatment with several antidepressant options were randomized to receive either iTBS or rTMS delivered to their left dorsolateral prefrontal cortex. They received the given treatment five days/week for four to six weeks.
Patients who received iTBS showed a nearly identical level of improvement in depression to those who received rTMS. Self-reports of pain intensity were worse among those who received iTBS, but the dropout rate was not higher for that group. Headaches were the most common side effect reported, and rates were similar across both groups. The authors judged iTBS to be a comparable, non-inferior alternative to rTMS for people with major depression.
Among participants who received iTBS, depression improved significantly, with 32 percent reporting a remission of depression symptoms. Those who received standard rTMS had a remission rate of 27 percent.