Adolescents with Bipolar Disorder May Have Higher Levels of Vitamin D–Binding Protein

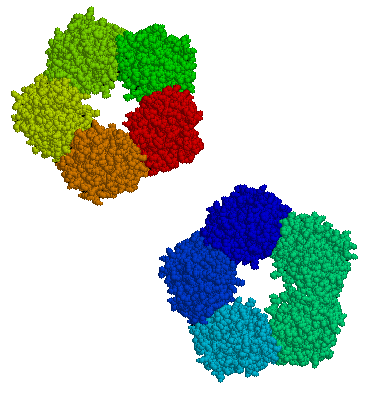
Vitamin D binding protein. Illustration: Emw [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]
A 2018 article by Brawnie Petrov and colleagues in the journal Translational Psychiatry suggests that adolescents with bipolar disorder have higher levels of vitamin D–binding protein than adolescents without a mood disorder. The researchers wrote that vitamin D–binding protein “responds early to cellular damage by binding…structural proteins and activating inflammatory cells.”
This pilot study suggests that measuring levels of vitamin D–binding protein could be a useful marker of bipolar disorder. The study was small, with only 12 participants who had bipolar disorder, 11 who had unipolar depression, and 13 with no mood disorder. The researchers hope to follow up with larger studies in adolescents and adults using blood that has already been collected from people with bipolar disorder.
Vitamin D–binding protein is not measured by a standard blood test. The study authors used a technique where they “fished” for inflammatory factors that might be linked to mood disorders. The researchers began by looking for a link between other inflammatory markers in the blood and bipolar disorder, which have repeatedly been found in other studies, but they did not find any such association. There also did not seem to be a link between bipolar illness and vitamin D levels in the blood, only vitamin D–binding protein levels.
It can be especially difficult to distinguish early bipolar disorder from unipolar depression, and if the results of this small study are replicated, a blood test might eventually help to identify people with bipolar disorder earlier.
Biomarker Suggests Which Patients With Depression Respond to Cognitive Behavior Therapy Versus SSRI
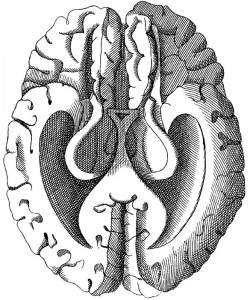
Not every treatment for mood disorders works for every patient, and for the 60% of depressed patients whose first treatment is ineffective, this wrong guess can translate into months of suffering, wasted money, lost productivity, and risk of suicide. An important trend in treatment research is the search for biomarkers, that is, biological indicators that can predict which patients might be likely (or unlikely) to respond to a particular treatment. A 2013 study by McGrath et al. in the journal JAMA Psychiatry suggests that brain glucose metabolism is one such biomarker.
Patients with untreated major depressive disorder had their brain glucose metabolism measured and then were randomized to receive 12 weeks of treatment either with the SSRI antidepressant escitalopram oxalate (trade name Lexapro) or with cognitive behavior therapy. Low glucose metabolism in a part of the brain called the anterior insula (compared to the rest of the brain) predicted that patients would reach remission on cognitive behavior therapy and respond poorly to escitalopram, while high metabolism in the same area predicted the opposite, that patients would reach remission while taking escitalopram and respond poorly to cognitive behavior therapy.
Researchers will want to test this finding with patients over the long term, but the data from this study suggest that anterior insula glucose metabolism may be a successful biomarker that can guide initial treatment selection for patients with depression.
Immune Response in Mania
While the reasons why one person develops bipolar disorder and another does not remain mysterious, the current thinking is that genes contribute some risk while immunological abnormalities contribute other risks. Researchers have identified certain antibodies whose levels spike during an episode of mania, as if the patient is having an immune reaction. These are referred to as biomarkers or inflammatory markers.
While various biomarkers for mania have been identified, until recently their effects had only been examined independently. A 2013 article by Dickerson et al. published in the journal PLOS ONE examined four biomarkers in combination. Each was a type of antibody: to the NR peptide of the NMDA receptor, to gliadin (a protein derived from gluten), to Toxoplasma gondii (a parasitic protozoan), and to Mason-Pfizer Monkey Virus. Measures of these four types of antibodies made up a combined inflammation score for participants in the study.
The study compared 57 patients presenting with a manic episode with 207 non-psychiatric controls and 330 patients who had had recent onset of psychosis, schizophrenia, or bipolar depression. The combined inflammation score of the mania group was significantly higher than the other groups at the time of hospital admission and at the time of evaluation several days later. It had returned to normal (i.e. not different from the other groups) at followup six months later, although those with the highest combined inflammation scores were at risk for re-hospitalization during that period.
The findings of this study suggest that hospitalization for mania is associated with immune activation, and the level of this activation predicts subsequent re-hospitalization. Treatments for mania that target this inflammatory response should be investigated.
BDNF Is Decreased in Depression and Mania
Brain-derived neurotrophic factor (BDNF), which protects neurons and is necessary for long-term memory, can be measured in blood. In a symposium on bipolar disorder at the 2012 meeting of the Society of Biological Psychiatry, researcher Flavio Kapsczinski reviewed evidence from several meta-analyses showing that low levels of BDNF in the blood correlate with severity of an episode of depression or mania. In addition to the findings that BDNF levels are low during a mood episode, there are other reliable biomarkers of illness, including increases in intracellular calcium, increases in cortisol and failure to suppress cortisol by dexamethasone, and a variety of indices of inflammation and oxidative stress.
There are several common variants of the gene responsible for the production of BDNF, depending on which types of amino acids appear in its coding—valine or methionine. The Val66Val allele of proBDNF is the most frequently occurring in the population, and is the best-functioning variant. Those with a methionine substitution (Val66Met or Met66Met) have less efficient forms of BDNF. Researcher Jair Soares reported that the Met allele was associated with deficits in declarative memory in patients with bipolar disorder, and was also associated with smaller volume of the anterior cingulate gyrus.
Researcher Ghanshyam N. Pandey reported that patients with pediatric or adult bipolar disorder had decreased BDNF protein and mRNA levels in platelets and lymphocytes compared to controls. Treatment significantly increased these BDNF levels in the pediatric, but not in the adult bipolar subjects. These measurements in blood are consistent with findings that there are decreases in BDNF in the hippocampus and prefrontal cortex of patients who died while depressed or who committed suicide compared to controls.
CRP in Blood Predicts Onset of New Episode in Childhood Mood Disorders
At the 2013 meeting of the International Society for Bipolar Disorders, researcher Barbara Gracious presented evidence that increased levels of high sensitivity c-reactive protein (hsCRP), a marker of inflammation, were associated with an increased risk for developing a full-blown mood episode in 71 youth (average age 13.8) participating in a study called Longitudinal Assessment of Manic Symptoms (LAMS-2). The children were selected for the study because they had manic symptoms that were not severe enough to meet criteria for a diagnosis of bipolar I or II disorder. This research has not yet been published in a peer-reviewed journal, but the abstract can be found in first 2013 supplement of the journal Bipolar Disorders (page 67).
CRP levels are also known to predict cardiovascular disease and Type II diabetes.
Levels of 25-OH vitamin D, TNF?, and IL-6 did not predict a later mood disorder.
Editor’s Note: These data suggest the importance of assessing CRP and other markers in youth who are either prodromal (having early symptoms of a mood disorder) or at high risk because of a family history of a mood disorder.
The next step for clinical research would be to determine what treatment might decrease CRP and whether it would also prevent the development of mood episodes.
Inflammatory Markers May Predict Antidepressant Response
There appears to be a link between inflammation and depression. In the journal Neuropsychopharmacology, Cattanes et al. reported in 2013 that compared to controls, depressed patients had significantly higher baseline levels of inflammatory cytokines, less glucocorticoid receptor function, less neuroplasticity, and fewer neuroprotective factors. Certain variables predicted response to treatment, others were seen only in responders, and still others changed in everyone with antidepressant treatment.
Higher baseline levels of inflammatory markers interleukin IB, macrophage inhibitory factor (MIF), and tumor necrosis factor TNF? were each associated with nonresponse to antidepressant treatment, and the three combined accounted for 50% of the variance in response—that is, they were the major predictor of whether a patient responded to treatment.
Levels of other factors changed in only those patients who responded well to antidepressants. The biggest changes were the normalization in levels of the neurotrophic factors BDNF and VEGF.
Several other markers normalized with antidepressant treatment regardless of whether the patients responded to treatment, and these included decreases in cytokines interleukin-IB and MIF and improved glucocorticoid receptor function.
The three different kinds of findings about these biomarkers were observed regardless of what type of antidepressant was used—SSRI versus tricyclic nortriptyline (which blocks norepinephrine reuptake).
Editor’s Note: This study replicates other studies in depression where signs of inflammation have been observed, including increases in inflammatory cytokines, decreases in glucocorticoid receptor function (needed to suppress high levels of the stress hormone cortisol) and lower levels of neuroplasticity and neuroprotection markers. This, however, is one of the first studies to show that levels of these markers at baseline may predict response to antidepressant treatment.
Also novel are the findings that while some high interleukin levels at baseline predicted antidepressant non-response, other ones normalized only in responders, and still others changed with treatment independent of whether the patients’ depression improved. These exciting findings require replication, but suggest the future possibility of personalized medicine, that is, choosing medications based on an individual biochemical marker profile. Eventually direct use of anti-inflammatory agents may be necessary in those with the highest levels of cytokines (predicting non-response to conventional antidepressant treatment). The same types of studies are needed in bipolar depression to determine the relationship between these inflammatory markers and treatment response.
Neurological Biomarkers May Eventually Predict Response to Antidepressants
 T.L. Lauriat reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that low baseline levels of the neurotransmitter GABA in the brains of depressed patients were associated with greater response to antidepressants. GABA was measured using magnetic resonance spectroscopy (MRS).
T.L. Lauriat reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that low baseline levels of the neurotransmitter GABA in the brains of depressed patients were associated with greater response to antidepressants. GABA was measured using magnetic resonance spectroscopy (MRS).
These data raise the possibility that easily observed neurobiological markers, such as levels of GABA or the neurotransmitter glutamate, may ultimately be helpful in predicting clinical response to particular treatments.
Biomarker Panel May Help Diagnose Major Depressive Disorder
It is hoped that measuring biochemical substances in blood will help in the diagnosis of mood disorders and help direct patients to the most effective therapeutic regimens. J.L. Billbielo reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that investigators from Ridge Diagnostics in North Carolina were using this type of biomarker panel in an attempt to provide a predictive algorithm for a diagnosis of major depressive disorder. The panel of 10 assays was derived from a larger screening set and included: alpha 1 antitrypsin (Alpha 1AT), brain-derived neurotrophic factor (BDNF), cortisol, epidermal growth factor (EGF), resistin, and soluble tumor necrosis factor receptor II (sTNFR2). The research group found that this optimized algorithm distinguished depressed subjects from normal controls with a sensitivity of approximately 90% and a sensitivity of 84%.
Editor’s note: This assay is available commercially and appears to represent an interesting panel of potential neurobiological markers of depression, including neurotrophic factors, endocrine stress hormones, and inflammatory markers. While its diagnostic utility is somewhat doubtful and must be further demonstrated, this editor hopes that similar panels could ultimately predict individual clinical response to a given treatment. For example, patients with high levels of inflammatory markers might respond better to treatments aimed at suppressing inflammation. Read more