IVIG Produces Long-Term Results in PANDAS
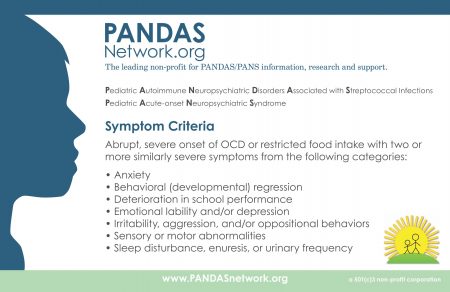
PANDAS, or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, is an autoimmune condition that produces psychiatric symptoms that appear suddenly following a case of strep throat in children. These symptoms can include obsessive-compulsive symptoms, tics, and behavioral dyscontrol and regression. Treatments are still experimental, but those that target the immune system are expected to be most successful at improving PANDAS.
In 2015, Miro Kovacevic and colleagues published a case series describing the use of intravenous immunoglobulin treatment (IVIG) in twelve children with PANDAS in the Journal of Child and Adolescent Psychopharmacology. One or in some cases two injections of IVIG brought about long-term remission in the children with PANDAS.
IVIG consists of a wide range of antibodies from multiple individuals delivered via injection. This increase in the quality or quantity of antibodies in the recipient is thought to suppress the production of antibodies that attack brain cells, causing PANDAS. The case series was based on patients at a large clinical practice that specializes in the treatment of PANDAS. The practice used a dosage of 1.5g/kg divided into two daily doses of 750 mg/kg, meant to match twice the volume of the patients’ own immunoglobulin G.
IVIG and other anti-inflammatory approaches are also effective in PANS, a more general variation on PANDAS in which psychiatric symptoms occur following an infection other than strep.
Antibody Sirukumab Improves Depression and Anhedonia in Patients with Rheumatoid Arthritis
Patients with rheumatoid arthritis have high levels of the inflammatory proteins known as interleukin-6 (IL-6), which have been implicated in depression and stress. Rheumatoid arthritis is sometimes characterized by depressive symptoms as well. New research by Dai Wang and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry suggests that treating the high levels of IL-6 in rheumatoid arthritis with the human anti–interleukin-6 antibody sirukumab can reduce symptoms of depression and anhedonia (loss of capacity to experience pleasure).
In the study, patients with rheumatoid arthritis and symptoms of depression or anhedonia were randomized to receive either placebo or sirukumab. After 12 weeks, those who received sirukumab had significantly reduced depression.
Editor’s Note: These data are consistent with meta-analyses showing that IL-6 is elevated in depression and with a study by Scott Russo showing that in animals, interfering with IL-6 blocks the development of depression-like behaviors that typically occur after repeated defeat stress (when an animal is subjected to attacks from a larger, more dominant animal).
Immune Response in Mania
While the reasons why one person develops bipolar disorder and another does not remain mysterious, the current thinking is that genes contribute some risk while immunological abnormalities contribute other risks. Researchers have identified certain antibodies whose levels spike during an episode of mania, as if the patient is having an immune reaction. These are referred to as biomarkers or inflammatory markers.
While various biomarkers for mania have been identified, until recently their effects had only been examined independently. A 2013 article by Dickerson et al. published in the journal PLOS ONE examined four biomarkers in combination. Each was a type of antibody: to the NR peptide of the NMDA receptor, to gliadin (a protein derived from gluten), to Toxoplasma gondii (a parasitic protozoan), and to Mason-Pfizer Monkey Virus. Measures of these four types of antibodies made up a combined inflammation score for participants in the study.
The study compared 57 patients presenting with a manic episode with 207 non-psychiatric controls and 330 patients who had had recent onset of psychosis, schizophrenia, or bipolar depression. The combined inflammation score of the mania group was significantly higher than the other groups at the time of hospital admission and at the time of evaluation several days later. It had returned to normal (i.e. not different from the other groups) at followup six months later, although those with the highest combined inflammation scores were at risk for re-hospitalization during that period.
The findings of this study suggest that hospitalization for mania is associated with immune activation, and the level of this activation predicts subsequent re-hospitalization. Treatments for mania that target this inflammatory response should be investigated.