IVIG Produces Long-Term Results in PANDAS
PANDAS, or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, is an autoimmune condition that produces psychiatric symptoms that appear suddenly following a case of strep throat in children. These symptoms can include obsessive-compulsive symptoms, tics, and behavioral dyscontrol and regression. Treatments are still experimental, but those that target the immune system are expected to be most successful at improving PANDAS.
In 2015, Miro Kovacevic and colleagues published a case series describing the use of intravenous immunoglobulin treatment (IVIG) in twelve children with PANDAS in the Journal of Child and Adolescent Psychopharmacology. One or in some cases two injections of IVIG brought about long-term remission in the children with PANDAS.
IVIG consists of a wide range of antibodies from multiple individuals delivered via injection. This increase in the quality or quantity of antibodies in the recipient is thought to suppress the production of antibodies that attack brain cells, causing PANDAS. The case series was based on patients at a large clinical practice that specializes in the treatment of PANDAS. The practice used a dosage of 1.5g/kg divided into two daily doses of 750 mg/kg, meant to match twice the volume of the patients’ own immunoglobulin G.
IVIG and other anti-inflammatory approaches are also effective in PANS, a more general variation on PANDAS in which psychiatric symptoms occur following an infection other than strep.
Immune Therapy with IVIG May Help Children with PANDAS
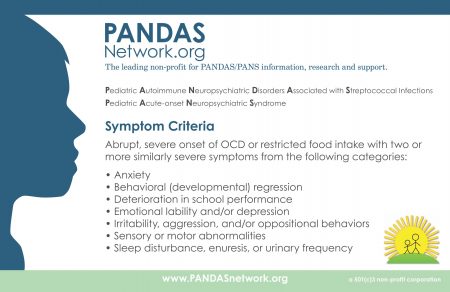
 A small number of children exposed to streptococcal bacteria have an autoimmune response that manifests in sudden, severe obsessive-compulsive behaviors and tics. This disorder is known as PANDAS: pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, and it resembles the broader disorder PANS, which can occur after other types of bacterial or viral infections.
A small number of children exposed to streptococcal bacteria have an autoimmune response that manifests in sudden, severe obsessive-compulsive behaviors and tics. This disorder is known as PANDAS: pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, and it resembles the broader disorder PANS, which can occur after other types of bacterial or viral infections.
Research on treatments for PANDAS and PANS is scant, but therapies that target the immune system seem to have more success than typical psychiatric treatments. In a 2015 article in the Journal of Child and Adolescent Psychiatry, researcher Miro Kovacevic and colleagues described a case series of 12 youths with PANDAS who were treated with intravenous immunoglobin (IVIG), a treatment designed to regulate the immune system. (The participants also met diagnostic criteria for PANS.)
The authors suggest that PANDAS symptoms result from a misdirected immune response that attacks the patient’s brain instead of or in addition to attacking the initial infection. IVIG treatment uses a mixture of antibodies from about 1,000 people. When this mixture is infused into the patient’s blood, the antibodies help deflect the autoimmune attack on the patient’s body. All of the 12 patients had a good long-term response to IVIG. Some did well after just one infusion, while two needed a second infusion because they did not respond to the first, and five had recurring symptoms that required a second infusion. All of the patients had previously received two other types of treatment: a 5-day course of steroids and antibiotics, neither of which produced immediate improvements.
The authors concluded that effective long-term treatment of PANS or PANDAS should combine immune therapy, prevention of future infections with antibiotics, and treatment that targets their psychiatric symptoms, such as anti-obsessional medication or cognitive-behavioral therapy.
Azithromycin Antibiotic May Help PANS
PANS is a neuropsychiatric syndrome characterized by the acute onset of obsessive compulsive and other abnormal behaviors, tics, and mood changes that appear in a child following a bacterial or viral infection. PANS refers to any pediatric acute-onset neuropsychiatric syndrome of this type, while PANDAS refers more specifically to such a syndrome that occurs after exposure to streptococcal infections.
New research suggests that treatment with the antibiotic azithromycin can treat PANS. In a study presented at the 2016 meeting of the Society of Biological Psychiatry, Tanya K. Murphy and colleagues found that among 32 children aged 4–14 who showed obsessive compulsive symptoms following an infection, those who were given a 4-week course of azithromycin (10mg/kg of body weight, up to 500 mg/day) saw a 26% drop in symptoms, compared to a 1% drop in symptoms in those who received placebo instead.
At the end of the four weeks, 38.9% of the azithromycin group were classified as much improved or very much improved, while no one in the placebo group achieved this level of improvement. Azithromycin treatment increased the QTc interval (a measure of heart rate) and pulse in the study participants, but did not have any other notable side effects.
PANS is thought to arise from an immune response to infection that goes awry and begins attacking neurons in the brain, particularly in the thalamus. For a more complete review of PANS, see several of our earlier articles about PANS and an excellent review article by researcher Kiki Chang and colleagues in the Journal of Child and Adolescent Psychopharmacology in 2015.
It is important to work up a child suspected of having PANS, as the syndrome does not usually respond to conventional psychiatric treatment and often requires anti-inflammatory drugs (steroids or immunosuppressants), intravenous immunoglobulin (IVIG), plasma exchange, the TNF alpha blocker infliximab, or antibiotics.
PANS: Sudden OCD or Restrictive Eating Disorder Onset Following an Infection
 At the 2014 meeting of the International Society for Bipolar Disorder, researcher Kiki Chang discussed Pediatric Acute Onset Neuropsychiatric Syndromes (PANS), a newly identified phenomenon in which children suddenly develop obsessive compulsive disorder (OCD) and/or a restrictive eating disorder following an infection or other process that stimulates an immune/inflammatory reaction in the brain. A similar phenomenon, Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS), was initially identified by Susan Swedo of the National Institute of Mental Health (NIMH) and refers to children (usually under 6–10 years old) who develop OCD and/or tics following a case of strep throat or scarlet fever.
At the 2014 meeting of the International Society for Bipolar Disorder, researcher Kiki Chang discussed Pediatric Acute Onset Neuropsychiatric Syndromes (PANS), a newly identified phenomenon in which children suddenly develop obsessive compulsive disorder (OCD) and/or a restrictive eating disorder following an infection or other process that stimulates an immune/inflammatory reaction in the brain. A similar phenomenon, Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS), was initially identified by Susan Swedo of the National Institute of Mental Health (NIMH) and refers to children (usually under 6–10 years old) who develop OCD and/or tics following a case of strep throat or scarlet fever.
PANS may have an autoimmune component. In addition to acute onset of OCD and eating restriction, other symptoms include mood episodes (depression, mania), high aggression/irritability, anxiety (particularly separation anxiety), cognitive problems (ADHD, handwriting regression), regressive behaviors, and somatic signs such as sleep difficulties and urinary urgency. Biological abnormalities may include: abnormalities in red blood cell sedimentation rate, elevated C-reactive protein (CRP), high Anti DNase B and/or Antistreptolysin O (ASO) titers (anti-Streptococcus antibodies), mycoplasma IgG or IgM antibodies (signs of some types of pneumonia), ANA (antinuclear antibodies, sign of an autoimmune disease), ferritin (a protein that stores iron), copper, and a panel of tests (the Cunningham Panel) by the company Moleculera Labs that measures antibodies for four neural antibodies (dopamine D1 receptors, dopamine D2 receptors, lysoganglioside (LysoGM-1), and tubulin) and calcium/calmodulin-dependent protein kinase activity (CaMKII).
PANS is three times more likely to affect males than females, and in the Stanford PANS Clinic sample of 50 youth, PANS was associated with strep infections (65%), mycoplasma bacteria (13%), viral or urinary tract infection (58%), and ear and other infections in 16%.
Symptoms included OCD (86%), anxiety (92%), mood disturbance (88%), and aggression (82%).
Treatments include steroids, the immunosuppressant mycophenolate, intravenous immunoglobulin (IVIG), plasma exchange, the tumor necrosis factor blocker infliximab, and sometimes the antibiotic amoxicillin.
Chang also described a case in which a 15-year-old developed minocycline-induced OCD and acute onset of severe mania that included urinary incontinence and was unresponsive to medication. The patient had elevated ANA, anti-thyroid antibodies, and reduced complement C4 proteins, along with elevated antibodies to dopamine D1 and D2 receptors, LysoGM-1, and tubulin.