IVIG Produces Long-Term Results in PANDAS
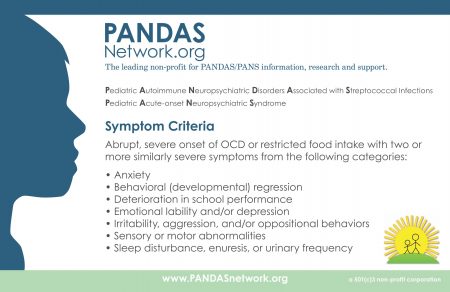
PANDAS, or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, is an autoimmune condition that produces psychiatric symptoms that appear suddenly following a case of strep throat in children. These symptoms can include obsessive-compulsive symptoms, tics, and behavioral dyscontrol and regression. Treatments are still experimental, but those that target the immune system are expected to be most successful at improving PANDAS.
In 2015, Miro Kovacevic and colleagues published a case series describing the use of intravenous immunoglobulin treatment (IVIG) in twelve children with PANDAS in the Journal of Child and Adolescent Psychopharmacology. One or in some cases two injections of IVIG brought about long-term remission in the children with PANDAS.
IVIG consists of a wide range of antibodies from multiple individuals delivered via injection. This increase in the quality or quantity of antibodies in the recipient is thought to suppress the production of antibodies that attack brain cells, causing PANDAS. The case series was based on patients at a large clinical practice that specializes in the treatment of PANDAS. The practice used a dosage of 1.5g/kg divided into two daily doses of 750 mg/kg, meant to match twice the volume of the patients’ own immunoglobulin G.
IVIG and other anti-inflammatory approaches are also effective in PANS, a more general variation on PANDAS in which psychiatric symptoms occur following an infection other than strep.
Azithromycin Antibiotic May Help PANS
PANS is a neuropsychiatric syndrome characterized by the acute onset of obsessive compulsive and other abnormal behaviors, tics, and mood changes that appear in a child following a bacterial or viral infection. PANS refers to any pediatric acute-onset neuropsychiatric syndrome of this type, while PANDAS refers more specifically to such a syndrome that occurs after exposure to streptococcal infections.
New research suggests that treatment with the antibiotic azithromycin can treat PANS. In a study presented at the 2016 meeting of the Society of Biological Psychiatry, Tanya K. Murphy and colleagues found that among 32 children aged 4–14 who showed obsessive compulsive symptoms following an infection, those who were given a 4-week course of azithromycin (10mg/kg of body weight, up to 500 mg/day) saw a 26% drop in symptoms, compared to a 1% drop in symptoms in those who received placebo instead.
At the end of the four weeks, 38.9% of the azithromycin group were classified as much improved or very much improved, while no one in the placebo group achieved this level of improvement. Azithromycin treatment increased the QTc interval (a measure of heart rate) and pulse in the study participants, but did not have any other notable side effects.
PANS is thought to arise from an immune response to infection that goes awry and begins attacking neurons in the brain, particularly in the thalamus. For a more complete review of PANS, see several of our earlier articles about PANS and an excellent review article by researcher Kiki Chang and colleagues in the Journal of Child and Adolescent Psychopharmacology in 2015.
It is important to work up a child suspected of having PANS, as the syndrome does not usually respond to conventional psychiatric treatment and often requires anti-inflammatory drugs (steroids or immunosuppressants), intravenous immunoglobulin (IVIG), plasma exchange, the TNF alpha blocker infliximab, or antibiotics.
Deep TMS May Reduce OCD Symptoms
Obsessive compulsive disorder (OCD) occurs in about 2% of the population worldwide. Selective serotonin reuptake inhibitor (SSRI) antidepressants are the most commonly used treatment for OCD, but not all patients respond adequately to them.
At the 2015 meeting of the Transcranial Magnetic Stimulation Society, researcher Joseph Zohar presented evidence that deep transcranial magnetic stimulation (deep TMS) targeted over the medial prefrontal cortex may reduce OCD symptoms. In TMS treatment, an electromagnetic coil is placed against the patient’s head and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain. In Zohar’s study, patients with OCD were randomized to receive deep TMS at frequencies of either 20 Hz or 1 Hz, or a sham procedure. The 20 Hz deep TMS resulted in a 28% reduction in OCD symptoms compared to the other two groups, indicating that the 20 Hz treatment had a large effect size.
In addition to the deep TMS procedures, all patients also received cognitive behavioral therapy, high doses of SSRIs, and relapse prevention training.
Editor’s Note: It is interesting that 20 Hz deep TMS, which activates the prefrontal cortex, was more effective than 1 Hz, which decreases activity there. Other attempts to treat OCD have focused on suppressing frontal-striatal-thalamic circuits, which are overactive in the disorder. Since the medial prefrontal cortex is an important area for the new learning required for the extinction of anxiety symptoms in a variety of disorders, increasing activity in this medial prefrontal target area with 20 Hz may activate that extinction process allowing new learning rather than nonspecifically suppressing hyperactive frontal-striatal-thalamic circuits as 1 Hz TMS would do.