Surface Area of Cortex Is Reduced After Multiple Manic Episodes
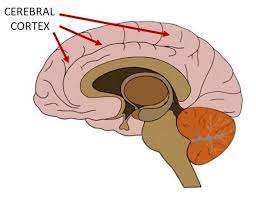
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.
Lumateperone Improves Bipolar Depression Symptoms
At a recent scientific meeting, Suresh Durgam of Intra-Cellular Therapies, Inc. reported on a study of lumateperone tosylate for the treatment of bipolar depression. Lumateperone tosylate is a mechanistically novel antipsychotic that has been approved by the US Food and Drug Administration for the treatment of schizophrenia.
In a double-blind, placebo-controlled study, the drug showed efficacy in bipolar I and II depression. In a 6-week study, 377 patients received either 42 mg/day of lumateperone or placebo, and 333 (87.4%) completed treatment. Lumateperone treatment significantly improved total scores on the Montgomery Asberg Depression Rating Scale (MADRS) compared with placebo. Item analysis revealed that 8 of 10 MADRS items improved significantly in comparison with placebo by day 29, and all items did by day 43. The largest effects were in reported sadness, apparent sadness, inner tension and reduced sleep. Durgam and colleagues concluded that lumateperone at a dose of 42mg improves a broad range of symptoms in bipolar I and bipolar II depression.
Saphris Reformulated for Kids with Bipolar I
The atypical antipsychotic asenapine has been reformulated for bipolar I disorder in children aged 10–17. The drug (trade name Saphris) was approved by the Food and Drug Administration (FDA) in 2009 for adults with schizophrenia and bipolar disorder. It is sometimes used as a treatment for mixed episodes (depression with some symptoms of mania).
The new formulation consists of 2.5mg tablets that are taken sublingually (under the tongue), and are available in a black cherry flavor. These can be prescribed as monotherapy for the acute treatment of manic or mixed episodes in children and teens.
Differences in Depressive Episodes Across Bipolar I, II, and Major Depression
 In a recent retrospective study, people with bipolar disorder I, bipolar disorder II, and major depressive disorder were interviewed about a 14-year period of their illness, and several differences emerged.
In a recent retrospective study, people with bipolar disorder I, bipolar disorder II, and major depressive disorder were interviewed about a 14-year period of their illness, and several differences emerged.
People with bipolar disorder I described their illnesses as including more psychomotor retardation (slowing of movements) and more psychotic features. People with bipolar disorder II had more mixed states than both people with major depression and people with bipolar I disorder. They also had less psychomotor slowing than people with bipolar I disorder.
Another purpose of this study by Andrew Frankland and colleagues in the Journal of Clinical Psychiatry, was to determine the effectiveness of the Probabalistic Approach to Bipolar Disorder, a statistical method for differentiating diagnoses. The approach was successful in differentiating both bipolar subtypes from major depression, but not in differentiating between the bipolar subtypes.
ADHD and Bipolar Disorder Are Inherited Separately
While attention-deficit hyperactivity disorder (ADHD) is fairly common among people with bipolar disorder, the genetic risks of inheriting these two illnesses run separately in families. In a recent study of 465 people and 563 of their first-degree relatives by Susan Shur-Fen Gau and colleagues, people with bipolar I disorder were likely to have relatives with bipolar I disorder, and people with ADHD were likely to have relatives with ADHD, but ADHD did not increase risk of bipolar disorder and vice versa.
The researchers hypothesize that other reasons people might develop both disorders include developmental precursors to the illnesses, neurocognitive functioning, sleep problems, and personality traits such as impulsivity and disinhibition.
Editor’s Note: At a recent scientific meeting, Gau and her colleague Kathleen Merikangas said that people with bipolar disorder in the study were five times more likely to have relatives with bipolar disorder. Bipolar disorder and ADHD were comorbid in 37.8% of those with bipolar I disorder, 16.4% in bipolar II disorder, 14% in depression, and 1.1% in normal controls.



