Surface Area of Cortex Is Reduced After Multiple Manic Episodes
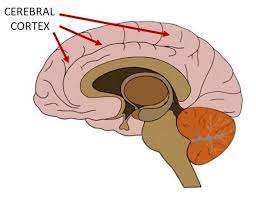
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.
Untreated Episodes of Bipolar Disorder Worsen Over Time, But Prevention is Possible
A 2017 literature review by researcher Lars V. Kessing and Per K. Andersen in the journal Acta Psychiatrica Scandinavica reports that the greater a patient’s number of previous episodes of bipolar disorder, the more likely that patient is to have a more difficult course of illness and poorer outcomes. The number of episodes was associated with more rapid recurrences, duration and severity of episodes, more automatic episodes (i.e. not triggered by stress), risk of dementia, treatment resistance, lack of recovery between episodes, and brain volume losses.
In an article in the journal Bipolar Disorders in 2016, BNN Editor-in-Chief Robert M. Post described the value of preventive treatment in reducing episodes and protecting the brain from the damage that accompanies them.
Given that episodes, stressors, and bouts of substance abuse can affect the way genes are transcribed via a phenomenon known as epigenetics, preventing these occurrences could lead to an easier course of illness and improved outcomes. Patients should provide their physicians with feedback about their response to prior medications and any side effects they experience over time so that their medication regime can be adjusted until it is maximally effective.
Patients with severe illness and multiple previous episodes may need a complex medication regimen that includes multiple types of medications that target different systems of neurotransmitters.
This philosophy of treatment is presented in several publications, including the 2008 book Treatment of Bipolar Illness: A Casebook for Clinicians and Patients by Post and Gabrielle Leverich, and more recently in the article “Treatment of Bipolar Depression: Evolving Recommendations” in the journal Psychiatric Clinics of North America. An open access article by Post, “New Perspectives on the Course and Treatment of Bipolar Disorders,” published in the journal Edizioni Minerva Medica S.p.A. in 2017, describes the need for early and sometimes complex combination therapy, including the non-intuitive idea that more medications (carefully prescribed) can actually produce fewer side effects than large doses of a single medication.
Another good resource for patients is a daily personal calendar that can be used to track ongoing symptoms, side effects, and response to medications. We offer several types of these calendars free here. My Mood Monitor, or What’s My M3, is a validated screening instrument that can detect depression, anxiety disorders, and mania in response to weekly self-reports. It is available online and as an app, and can be used to track illness course and response to treatment.
Antipsychotics That Worked for A First Episode May Not Work As Well a Second Time
 In new research by Ofer Agid and colleagues, patients in their first schizophrenic episode who reached remission in response to one of two antipsychotic medications (risperidone or olanzapine) and relapsed due to medication non-adherence were re-treated with the same medication regimen that had brought about remission. Reinitiating the same treatment was not as successful in bringing about remission of the patients’ second psychotic episodes.
In new research by Ofer Agid and colleagues, patients in their first schizophrenic episode who reached remission in response to one of two antipsychotic medications (risperidone or olanzapine) and relapsed due to medication non-adherence were re-treated with the same medication regimen that had brought about remission. Reinitiating the same treatment was not as successful in bringing about remission of the patients’ second psychotic episodes.
Patients showed different types of trajectories in their first remission, from immediate to gradual improvement, and these predicted parallel trajectories of their treatment response during the second episode, though the muted response to antipsychotics existed across the board. Dopamine is the main target of antipsychotic treatments, but its role in schizophrenia is not straightforward, and Agid and colleagues stress that response and relapse are multidimensional processes.
Editor’s Note: These data are consistent with the research of J.A. Lieberman and colleagues fifteen years ago, which showed that response to antipsychotic treatment is poorer in successive episodes of psychosis. The findings are also consistent with the idea of episode sensitization in mood disorders, developed by this author (Robert Post). Episode sensitization refers to the case in which greater numbers of prior depressions or manias are associated with faster relapse and a greater degree of treatment resistance.
The data raise major doubts about the common practice of quitting medications to see if remission can be maintained without them. There are dozens of studies in patients with schizophrenia showing that continuous treatment is more effective than intermittent treatment.
More Evidence That Lithium Prevents Mania and Depressions
There is a large body of research showing that lithium is better than placebo and a variety of comparison drugs at preventing manic episodes in people with bipolar disorder. It has been less clear whether lithium is as effective in preventing depressions in bipolar patients. In a 2014 meta-analysis in the International Journal of Bipolar Disorders, Emanuel Severus and colleagues confirmed that lithium was more effective than placebo at preventing mood episodes overall and manic episodes. In a fixed effect statistical analysis, lithium was also better at preventing depressive episodes.
The portion of the meta-analysis comparing lithium to placebo included seven randomized controlled trials that included a total of 1,580 patients. Lithium was more likely than placebo to lead to patients dropping out of a study for reasons other than a mood episode, but patients who received lithium were more likely to complete their clinical trials.
Another part of the meta-analysis compared lithium to anticonvulsant drugs. Seven trials were included totaling 1,305 patients. Lithium was better than anticonvulsants at preventing manic episodes, but equally effective at preventing mood episodes overall and depressive episodes specifically. There was also no difference in patients dropping out of the trials or completing the trials.
The researchers concluded that lithium remains the most valuable treatment option for bipolar disorder, because no other drug has such consistent efficacy in preventing manias and depressions and mood episodes in general.



