Meta-Analysis Shows Anti-Inflammatory Treatments Improve Bipolar Depression
 It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
It has been clear for some time that depression and inflammation are linked. This has led researchers to explore a variety of anti-inflammatory agents to treat depression. A meta-analysis of studies examining anti-inflammatory treatments for bipolar depression was published in the journal Bipolar Disorders in 2016.
Researcher Joshua D. Rosenblat and colleagues identified eight randomized controlled trials that met their criteria for anti-inflammatory treatments of bipolar disorder. These treatments included nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen and aspirin), omega-3 fatty acids, the antioxidant N-acetylcysteine, and pioglitazone (used to treat diabetes). Overall, the anti-inflammatory treatments had a moderate and statistically significant antidepressant effects. No serious side effects were reported, and the anti-inflammatory treatments did not cause a switch into mania in any of the participants.
The diversity of the anti-inflammatory treatments reviewed in this meta-analysis limit the extent to which it can be interpreted, but it is clear that more research on anti-inflammatory treatments for bipolar depression is needed. An open question is whether patients with particularly elevated levels of inflammatory markers in their blood would respond better to these anti-inflammatory treatments.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
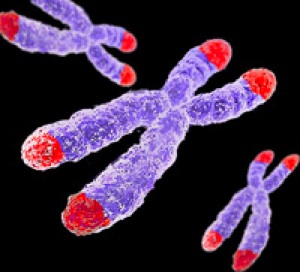
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
Clarifying the Effects of a Diabetes Drug that Improves Bipolar Depression
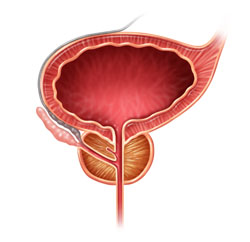
Research continues on pioglitazone, a drug typically used to treat diabetes but with other positive effects on depression and stroke risk. Some researchers are working on determining whether the drug increases the risk of developing certain cancers, including bladder, prostate, and pancreatic cancers. A recent study by James D. Lewis and colleagues in the journal JAMA found no statistically significant increase in risk of bladder cancer among patients taking the drug, but the researchers said they also couldn’t rule out that the drug may increase this risk, as has been seen in previous studies. The study by Lewis did show an increase in pancreatic and prostate cancers in patients taking pioglitazone, but the researchers did not determine whether this was caused by the drug.
Another recent study by Walter N. Kernan and colleagues in the New England Journal of Medicine reported that pioglitazone reduced the incidence of stroke and heart attack in patients with a history of stroke or blocked blood vessels in the brain but without a diagnosis of diabetes. Patients who received pioglitazone also experienced side effects including weight gain, edema (an increase in fluids in the body’s tissues) and serious bone fractures.
Pioglitazone has had positive effects in bipolar depression and may one day be used as a treatment for bipolar disorder. For now, it may be worthy of consideration for the treatment of diabetes in patients who also have bipolar depression.
Diabetes Drug Pioglitazone May Improve Bipolar Depression
The hypoglycemic drug pioglitazone is typically used to treat diabetes, but a 2015 study by A. Zeinoddini and colleagues shows that it may improve depressive symptoms in patients with bipolar disorder who do not have type 2 diabetes or the metabolic syndrome (characterized by high weight, cholesterol, triglycerides, and blood pressure).
Forty-four patients with bipolar disorder and a major depressive episode were randomized to receive either 30 mg/day of pioglitazone or placebo as an adjunctive treatment to lithium. Depressive symptoms were lower in the pioglitazone group at weeks 2, 4, and 6 of the six-week study.
No serious side effect occurred in the study, but pioglitazone use is associated with some risks in those using it for diabetes treatment. People taking pioglitazone for longer than a year have shown increased rates of bladder cancer. There is an increased risk of fractures of the upper arms, hands, and feet in female patients. The drug lowers blood sugar, but not enough to be a problem in people not taking other drugs that lower blood sugar. Pioglitazone can also cause fluid retention, worsening congestive heart failure. It can also cause mild weight gain, anemia, and sinus problems.