Optimum Lithium Levels
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Willem Nolen discussed optimal lithium levels to prevent episodes of bipolar disorder. Based on the limited number of controlled trials that have examined this issue and a survey of experts in the field, Nolen concluded that the standard dosing target to prevent bipolar episodes would be a blood concentration of 0.6 to 0.8 mEq/liter. This concentration could be dropped to 0.4 to 0.6 mEq/liter for patients who responded well to a higher dosage but needed to reduce side effects, and the concentration could be increased to 0.8 to 1.0 mEq/liter for patients who tolerated lithium treatment but showed an inadequate response.
There was no consensus as to optimal blood concentrations of lithium to prevent bipolar episodes in children and adolescents, but some researchers endorsed the same standard recommended for adults. For elderly patients, the majority of researchers recommended a slightly lower concentration of 0.4 to 0.6 mEq/liter, with the option to increase to a maximum of 0.8 mEq/liter in those under age 80 and 0.7 mEq/liter in those over age 80.
Lithium Reverses Some White Matter Abnormalities in Youth with Bipolar Disorder
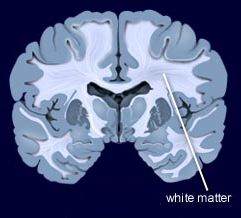 Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Editor’s Note: This is another reason to consider the use of lithium in children with bipolar disorder. Lithium treatment may help normalize some of the earliest signs of neuropathology in the illness.
Lithium FDA-Approved for Bipolar Disorder in Children 7–17
 In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
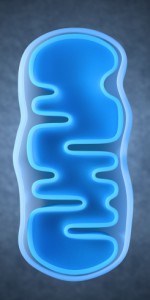
Mounting Evidence of Mitochondrial Dysfunction in Bipolar Disorder
At the 2019 meeting of the International Society for Bipolar Disorders, researchers Ana Andreazza, Olivia Dean and colleagues reviewed substantial data that implicate mitochondrial dysfunction in the mood and energy fluctuations that make up bipolar disorder. Most of the neurobiological alterations known to occur in bipolar disorder have a relationship to mitochondria, which produce energy within cells. These alterations include abnormalities in glutamate, gene expression, apoptosis (cell death), oxidative stress, low ATP (a molecule that stores energy), altered ion pumps, increased intracellular calcium, and insufficient glutathionine (an antioxidant made up of three amino acids).
Coenzyme Q10 is a mitochrondrial enhancer of Complex I, an enzyme that is key to the first step in mitochondrial energy production. A 2018 controlled study by Maryam Mehrpooya and colleagues published in the Journal of Clinical Psychopharmacology found that 200mg/day of CoQ10 was more effective than placebo at reducing symptoms of bipolar depression when added to patients’ stable treatment regimens that included mood stabilizers and antidepressants. The effect size was large (0.87), and it took eight weeks for the benefit over placebo to appear. Response rate to CoQ10 was 72% compared to 12% to placebo.
Editor’s Note: Some formulations of CoQ10 do not cross the blood-brain barrier easily, so only a very small percentage of the CoQ10 gets into the brain. Thus, consumers should be careful about the type of product they purchase. The one made by Takeda Pharmaceutical Company is likely to be effective.
Early Predictors of Suicide and Lithium as an Anti-Suicide Drug
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
Editor’s Note: Among all psychotropic drugs, lithium has the best data supporting its anti-suicide effects, both at therapeutic doses in patients with bipolar disorder and at trace levels in the water supply in the general population. People who live in locations where more lithium is naturally present in the water supply have lower rates of suicide than those who live in places with less lithium in the water. Malhi also noted that the antioxidant N-acetylcysteine (NAC), which has positive effects on mood and habitual behaviors, can reduce the incidence of lithium-induced dysfunction of the kidneys.
Treating Bipolar Depression in an Adolescent
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Ben Goldstein discussed a case of a 15-year-old with bipolar depression and his recommended treatments for the adolescent. Goldstein endorsed the use of an atypical antipsychotic such as lurasidone, and perhaps also quetiapine. Goldstein noted 2015 findings from researcher Robert Findling that lamotrigine was significantly more effective than placebo in adolescents 13–18 years old, but was not effective in those aged 10–12.
(In adults, researcher John Geddes and colleagues found that in patients with an inadequate antidepressant response to quetiapine, the addition of lamotrigine was more effective than adding a placebo, both acutely and in long-term follow-up. The only caveat was that lamotrigine was less effective in those who were also being treated with folate.)
Editor’s Note: Some other treatments could augment the effects of the regimen proposed by Goldstein, including lithium and the antioxidant N-acetylcysteine, which, it should be noted, takes more than eight weeks to become effective. Vitamin D3 could also be considered, as it is often low in children with psychiatric disorders. One treatment that went unmentioned at the meeting was repeated transcranial magnetic stimulation, or rTMS, which is effective and well-tolerated in adolescents with depression.
For patients with more rapidly cycling bipolar disorder and only partial response to medications, the combination of the ‘three Ls’ (lurasidone, lamotrigine, and lithium) could have considerable appeal, given that each drug is from a different class of medications, has a different mechanism of action, targets a different mood phase, and is relatively well-tolerated both alone and in combination with other drugs.
Newly Identified Effects of N-Acetylcysteine
 In a talk at the 2019 meeting of the International Society for Bipolar Disorders, researcher Michael Berk, who was responsible for some of the initial findings on the effects of the antioxidant N-acetylcysteine (NAC), summarized some of the newer findings about the treatment.
In a talk at the 2019 meeting of the International Society for Bipolar Disorders, researcher Michael Berk, who was responsible for some of the initial findings on the effects of the antioxidant N-acetylcysteine (NAC), summarized some of the newer findings about the treatment.
NAC has been found to be effective in bipolar depression and in the treatment of both positive and negative symptoms of schizophrenia. It also helps in the avoidance of cocaine, alcohol, tobacco, and marijuana. It can reduce habitual behaviors such as gambling, obsessive compulsive disorder (OCD), and trichotillomania (compulsive hair-pulling) and irritability and motor stereotypy (repeated movements) in autism.
A 2016 study by researcher Sudie E. Back and colleagues in the Journal of Clinical Psychiatry found that NAC improved symptoms of post-traumatic stress disorder (PTSD) in veterans who also had depression and substance use disorders at a dosage of 2.4 grams/day.
According to Berk, NAC also reduces the incidence of lithium-related renal failure and reduces mitochrondrial toxicity. One study reported that it improved working memory in patients with schizophrenia.
In his talk, Berk also noted that statins offer an interesting new avenue for treatment. Several studies have suggested statins can improve mood or reduce the likelihood of a depressive recurrence. Angiotension-active drugs (inhibitors) have also been reported to decrease the incidence of depression and to improve cognition.
Obesity Associated with Inflammation and Brain Abnormalities
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David J. Bond reviewed the data on the multiple adverse effects of obesity in patients with bipolar disorder. These include increased cardiovascular risk, poorer response to treatment, brain abnormalities, and decreased cognitive function, which is correlated with the degree of overweight.
Editor’s Note: These data emphasize the importance of starting a nutritious diet early in life and sustaining it through adulthood, avoiding the drugs most associated with weight gain such as clozapine and olanzapine, and facilitating weight loss with drugs. There are several treatments that can aid in weight loss. One is the diabetes treatment metformin, starting at a high dose of 500mg twice daily, and increasing to 1000mg twice daily if tolerated. The anticonvulsants topiramate or zonisamide also promote weight loss. The most effective option is a combination of the antidepressant bupropion sustained release (at a dose of 150–300mg) plus the anti–substance abuse drug naltrexone (50mg). This combination was associated with a loss of 10% of body weight over 12 weeks in women with diabetes.
Study in Mice Suggests that Compound in Turmeric May Reduce Anxiety and Promote Resilience to Stress
 Chronic stress is a risk factor for the development of mood and anxiety disorders. Researchers have begun to focus on how to promote resilience to stress. Curcumin is a micronutrient found in turmeric that has anti-inflammatory and antidepressant effects and may promote such resilience.
Chronic stress is a risk factor for the development of mood and anxiety disorders. Researchers have begun to focus on how to promote resilience to stress. Curcumin is a micronutrient found in turmeric that has anti-inflammatory and antidepressant effects and may promote such resilience.
Researchers studying human depression often design studies to see how mice with chronic social defeat stress respond to various interventions. Mice who are repeatedly menaced by a larger mouse begin to show symptoms that resemble human depression, such as social avoidance, lack of interest in saccharin compared to plain water (a stand-in for loss of enjoyment or anhedonia in humans), and anxiety.
In a 2018 article in the journal Neuropsychopharmacology, researcher Antonio V. Aubry and colleagues described the effects of curcumin on mice undergoing chronic social defeat stress. Mice who were given a diet that consisted of 1.5% curcumin showed a 4.5-fold increase in resilience to social defeat stress, measured by their performance during a test of social interaction. Among the 129 mice in the study, 64% showed the increase in resilience, the remaining 36% did not respond to the curcumin diet and had the normal ‘depressed’ response. The mice who responded well to curcumin released less of the stress hormone corticosterone, and they also had lower levels of the inflammatory marker IL-6.
All of the mice on the curcumin diet showed reduced anxiety during tests that forced them to travel through open spaces (when they prefer to stay in more enclosed spaces or move along the edges of an enclosure).
Red Meat Interacts with Bacteria in the Gut to Raise Heart Disease Risk
 A 2018 study by a group of researchers at the Cleveland Clinic have clarified the way that a diet heavy in red meat may lead to heart disease. The research centers on trimethylamine N-oxide (TMAO), a gut bacteria byproduct that is formed during digestion. When gut bacteria digest choline, lecithin, and carnitine, nutrients that are common in certain animal products and red meat, TMAO is produced.
A 2018 study by a group of researchers at the Cleveland Clinic have clarified the way that a diet heavy in red meat may lead to heart disease. The research centers on trimethylamine N-oxide (TMAO), a gut bacteria byproduct that is formed during digestion. When gut bacteria digest choline, lecithin, and carnitine, nutrients that are common in certain animal products and red meat, TMAO is produced.
In an article by Robert A. Koeth and colleagues in the European Heart Journal, the researchers show that diets that rely on red meat as the main protein source lead to more circulating TMAO than diets in which white meat or something other than meat is the primary source of protein. They found that in people who eat a lot of red meat, the kidneys are less efficient at expelling TMAO, and levels creep even higher. High levels of TMAO have been linked to hardening and narrowing of the arteries (atherosclerosis) and heart disease complications. High levels of TMAO in the blood can be a predictor of heart attack, stroke, and death.
The study of 113 participants consisted of three different diets that each participant followed in random order (with a washout period in between each diet). A month of eating a diet in which red meat was responsible for at least 25% of participants’ daily calories led to higher levels of TMAO in the blood and urine. TMAO increased threefold during the red meat diet periods compared to periods in which white meat or non-meat protein were the source of those calories, and in certain participants, TMAO increased as much as tenfold. When participants stopped eating the red meat diet, their TMAO levels fell over the following month.