Mounting Evidence of Mitochondrial Dysfunction in Bipolar Disorder
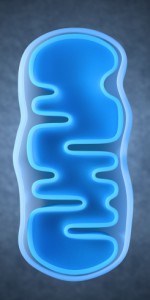
At the 2019 meeting of the International Society for Bipolar Disorders, researchers Ana Andreazza, Olivia Dean and colleagues reviewed substantial data that implicate mitochondrial dysfunction in the mood and energy fluctuations that make up bipolar disorder. Most of the neurobiological alterations known to occur in bipolar disorder have a relationship to mitochondria, which produce energy within cells. These alterations include abnormalities in glutamate, gene expression, apoptosis (cell death), oxidative stress, low ATP (a molecule that stores energy), altered ion pumps, increased intracellular calcium, and insufficient glutathionine (an antioxidant made up of three amino acids).
Coenzyme Q10 is a mitochrondrial enhancer of Complex I, an enzyme that is key to the first step in mitochondrial energy production. A 2018 controlled study by Maryam Mehrpooya and colleagues published in the Journal of Clinical Psychopharmacology found that 200mg/day of CoQ10 was more effective than placebo at reducing symptoms of bipolar depression when added to patients’ stable treatment regimens that included mood stabilizers and antidepressants. The effect size was large (0.87), and it took eight weeks for the benefit over placebo to appear. Response rate to CoQ10 was 72% compared to 12% to placebo.
Editor’s Note: Some formulations of CoQ10 do not cross the blood-brain barrier easily, so only a very small percentage of the CoQ10 gets into the brain. Thus, consumers should be careful about the type of product they purchase. The one made by Takeda Pharmaceutical Company is likely to be effective.
Antioxidant Supplement Coenzyme Q10 Looks Promising for Bipolar Depression
Coenzyme Q10 (CoQ10) is an antioxidant that occurs naturally in the human body, but its levels decline with age, medical illness, and depression. In a randomized, controlled trial that was published in the Journal of Clinical Psychopharmacology in 2018, researcher Maryam Mehrpooya and colleagues found that adding coenzyme Q10 supplements to a treatment regimen improved bipolar depression compared to adding placebo.
The pathophysiology of bipolar disorder involves mitochondrial dysfunction, oxidative stress, and inflammation, and coenzyme Q10 can affect all of these pathways. It is also neuroprotective, and may help prevent the degeneration of neurons in people with Alzheimer’s, Parkinson’s, or Huntington’s diseases.
The study included a final total of 69 participants who were randomly assigned to receive either 200 mg/day of coenzyme Q10 supplements or placebo in addition to their normal treatment regimen, which had been stable for at least two months at the time of the study. Participants’ bipolar depression was rated at the beginning of the study, after four weeks, and after eight weeks. At the eight-week mark, coenzyme Q10 showed a statistically significant benefit over placebo with a large effect size. Three participants who received coenzyme Q10 experienced full remission of their depression, and 72% of those in the coenzyme Q10 group improved compared to only 12% of those who received placebo.
The study had some limitations. It was small, and twenty participants dropped out of the study before its completion, which may have inflated the findings.
Previous research found that coenzyme Q10 had benefits in specific populations. In two non-blind studies (studies in which participants know that they are receiving the treatment in question rather than possibly a placebo), 29 older patients with bipolar disorder improved when taking 800 mg to 1200 mg/day of coenzyme Q10. A randomized, controlled trial of coenzyme Q10 in people with multiple sclerosis and depression found that 500 mg/day reduced fatigue symptoms and depression. Coenzyme Q10 has also improved well-being and energy in small, controlled trials in people with breast cancer, Gulf War veterans, and elderly populations.
Taking coenzyme Q10 is low-risk. It had no adverse effects in the study by Mehrpooya and colleagues. Gastrointestinal reactions are possible, but can be managed by taking coenzyme Q10 with food and spreading out dosing throughout the day. Insomnia is also possible, but is less likely when coenzyme Q10 is taken early in the day. One effect to note is that coenzyme Q10 can interact badly with the blood-thinner warfarin.
Editor’s Note: The study by Mehrpooya and colleagues is interesting. Another antioxidant, N-acetylcysteine (NAC), also took 2 months to work in trichotillomania and bipolar depression, so patients should be warned not to expect a quick response with either coenzyme Q10 or NAC. Other potentially useful supplements include: Vitamin D3 (1500–5000 IU/day), folate or L-methylfolate, and acetyl-L-carnitine. Acetyl-L-carnitine may work more quickly, based on its presumed mechanism (increasing the production of the inhibitory metabotrophic glutamate receptor mGluR-2, which inhibits glutamate release).