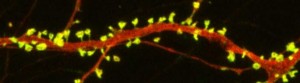
Lithium May Work by Restoring Dendritic Spines
New research on mice clarifies lithium’s effects on neurons and suggests how it can lead to improved symptoms. Dendrites are the long projections on neurons that seem to reach out to form synapses with other neurons. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. A 2016 article by research Ben Cheyette and colleagues in the journal Molecular Psychiatry reports that in mice with a genetic mutation common to people with autism, schizophrenia, and bipolar disorder, lithium restored healthy numbers of the mushroom-shaped spines. The lithium treatment also reversed symptoms such as lack of interest in social interactions, lack of motivation, and anxiety in the mice.
Cheyette and colleagues first identified a genetic mutation that affects signaling in what is known as the brain’s Wnt pathway. The mutation, while rare, is 80% more common in people with bipolar disorder, autism, and schizophrenia than in people without these disorders.
When the mice were given a similar mutation, they exhibited symptoms such as anxiety, decreased sociability, and lack of motivation. They also had reduced numbers of dendritic spines and impaired Wnt signaling.
Lithium can improve Wnt signaling by blocking an enzyme called GSK-3 beta that impairs the signaling.
Treating the mice with lithium restored their dendritic spines and improved their behavior.
Wnt signaling and dendritic spines may offer the key to lithium’s success in treating a variety of psychiatric disorders in people.
Preventative Treatment Should Begin After First Manic Episode
Evidence from multiple studies has indicated the importance of beginning preventative treatment, particularly with lithium, early in the course of bipolar disorder. A 2016 comprehensive literature review by researcher Katie Joyce and colleagues in the International Journal of Bipolar Disorders concluded that psychoeducation and medication are more effective in bipolar disorder when applied in earlier stages of the illness rather than later stages.
Several studies suggest that treatment for bipolar disorder should be started specifically after the first manic episode.
A 2014 study by researcher Lars Kessing and colleagues in the British Journal of Psychiatry examined 4,700 patients treated with lithium in Denmark. Kessing and colleagues found that those who started treatment after one manic episode were less likely to find lithium ineffective than those who started later.
Another study by researcher Michael Berk and colleagues presented at the International Society for Bipolar Disorders found that after a first manic episode, a year of treatment with lithium was much more effective on all measures of outcome, including mania and depression ratings, brain imaging, and neuropsychological functioning, than a year when patients were randomized to quetiapine (Seroquel).
Researcher Lakshmi Yatham and colleagues presented research at the International Society for Bipolar Disorders showing that patients recovered from the neuropsychological deficits associated with a first episode of mania if they were well treated and had no further episodes, while those who had new episodes did not return to their baseline capabilities. This suggests that early treatment that prevents future episodes helps maintain a healthy brain.
Kessing and colleagues previously reported in the British Journal of Psychiatry in 2013 that patients randomized to two years of treatment in an outpatient clinic specializing in mood disorders following a first hospitalization for mania had 40% fewer recurrences of bipolar episodes over the next six years than those who received treatment as usual. These data indicate that early treatment, which may include psychotherapy, medications, mood charting (i.e. keeping a daily record of symptoms) and illness education, can improve the long-term course of illness. Lithium is often a key component of such treatment.
Editor’s Note: This type of intensive, ongoing treatment is not the norm after a first manic hospitalization in the United States, but it should be. Given the new data on the impact of starting lithium after a first episode of mania, and lithium’s superiority over quetiapine in the year following a first episode, lithium treatment should be standard following a diagnosis of bipolar disorder.
In the past, sometimes doctors have recommended waiting until a patient has had multiple episodes of mania before beginning preventative treatment with lithium. This now appears to be a mistake.
Lithium protects against depressive as well as manic recurrences, and there is also evidence that it increases hippocampal and cortical volume, helping prevent cognitive deterioration in those with mild cognitive impairment. Lithium is also the most effective mood stabilizer for preventing suicide, and it increases the length of telomeres (caps on the end of DNA strands), thus preventing a wide range of medical and psychiatric illnesses. Lithium may need to be combined with other drugs to achieve a complete remission, but using it after a first mania is a good place to start.
Microdoses of Lithium May Stabilize Cognition in People with Alzheimer’s
Several researchers have found that lithium has some value in fighting dementia. The researcher Lars Kessing has published several studies showing that people taking clinical doses of lithium for bipolar disorder have a lower incidence of dementia in old age.
In 2011, another researcher, Oreste Vicentes Forlenza, reported that a year of low-dose lithium (typically around 300mg/day) slowed deterioration in people with mild cognitive impairment compared to placebo.
In an article published in the journal Current Alzheimer Research in 2013, researchers led by Marielza Andrade Nunes reported that very small doses of lithium (more than a thousand times lower than doses used to treat mood disorders) also improved mild cognitive impairment in people with Alzheimer’s disease.
In Nunes’ study, participants with Alzheimer’s disease were randomly assigned to receive either 300 micrograms of lithium daily or a placebo. Beginning at three months of treatment, those receiving the microdoses of lithium showed stable performance on a common Alzheimer’s evaluation tool that measures how well patients remember, recall information, and follow directions; while those taking placebo got worse.
This continued over the 15 months of the study, with the difference between the two groups intensifying over time—those taking placebo got worse, while those getting the microdoses of lithium remained stable.
There were no complaints of side effects from the microdoses of lithium, and participants showed no sign of impairment to their kidney or thyroid function (a risk with the higher doses of lithium used to treat bipolar disorder).
In 2015, Nunes and colleagues reported in the journal PLOS ONE that in a mouse model of Alzheimer’s disease, mice treated with chronic low doses of lithium in their water had less memory disruption, fewer plaques in the brain, and fewer reductions in cortex and hippocampus size compared to mice given plain water.
These studies suggest that low or micro doses of lithium may be a promising treatment for Alzheimer’s disease. Much more research is needed to determine appropriate lithium dosing for the treatment of dementia or cognition problems.
Lithium Increases Cortical Thickness in People with Bipolar Disorder
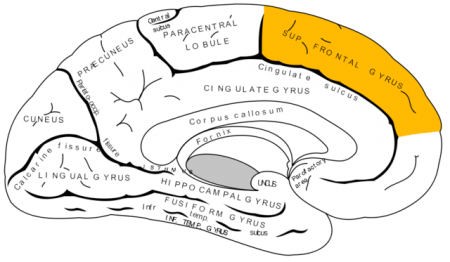 Recent studies have indicated that bipolar disorder is associated with changes to brain volume, including thinning of the cortex. In research presented at the 2016 meeting of the Society of Biological Psychiatry, researcher Noha Abdel Gawad reported that four weeks of lithium treatment increased cortical thickness in the left superior frontal gyrus. This is the third replication of this finding.
Recent studies have indicated that bipolar disorder is associated with changes to brain volume, including thinning of the cortex. In research presented at the 2016 meeting of the Society of Biological Psychiatry, researcher Noha Abdel Gawad reported that four weeks of lithium treatment increased cortical thickness in the left superior frontal gyrus. This is the third replication of this finding.
Other research has established that lithium treatment also increases the volume of the hippocampus in people with bipolar disorder. Together the findings provide strong evidence that lithium treatment protects neurons and can reverse brain changes associated with bipolar disorder.
Lithium Lengthens Telomeres
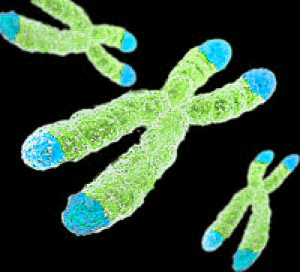 Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect the DNA as it is replicated. Depressive episodes and age can reduce the length of telomeres. Lithium treatment increases telomere length. At the 2016 meeting of the Society of Biological Psychiatry, researcher Martin Schalling reported that the longer a patient takes lithium, the more their telomere length increases.
Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect the DNA as it is replicated. Depressive episodes and age can reduce the length of telomeres. Lithium treatment increases telomere length. At the 2016 meeting of the Society of Biological Psychiatry, researcher Martin Schalling reported that the longer a patient takes lithium, the more their telomere length increases.
According to Schalling, people who respond well to lithium treatment show greater increases in telomere length than those who respond poorly to lithium.
While some cancers are associated with long telomeres, lithium use has not been found to increase cancer risk. In fact, lithium treatment can decrease the risk of certain cancers of the gastrointestinal, respiratory, and endocrine systems.
Lithium Treatment Reduces Inflammation, Mania-Like Behavior in Rats
Patients with bipolar disorder often show increases in signs of inflammation, including levels of the proteins IL-2, IL-4, Il-6, IL-10 and tumor necrosis factor in their blood. Lithium is the most effective treatment for bipolar disorder, but it is not yet clear how it works. A recent study by researcher Joao de Quevado and colleagues determined that lithium can reduce the same inflammatory markers in rats.
Rats were treated with amphetamine to induce mania-like behavior, which was accompanied by increases in some of the same inflammatory markers in the blood and brain that are increased in people with bipolar disorder. Lithium treatment reduced both the manic behavior and levels of these inflammatory proteins in the rats.
The researchers concluded that lithium may treat mania by reducing inflammation.
Lithium Improves Medical Outcomes
Lithium is one of the most effective medications for bipolar disorder, but it has other benefits as well. At a 2015 scientific meeting, Ronald Fieve reported that among 1021 psychiatric outpatients, 570 who received long-term lithium treatment for their psychiatric illnesses had a significantly lower likelihood of certain medical conditions compared to the other outpatients who did not receive lithium therapy. The medical conditions that lithium made less likely were seizures, amyotrophic lateral sclerosis (ALS) or Lou Gehrig’s disease, dementia, and heart attack.
It is not yet know how lithium decreases these medical conditions. It may be by increasing the length of telomeres. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with stressors or psychiatric illnesses. Lithium directly increases the enzyme telomerase, which maintains telomere length. This may be one reason lithium use provides some protection from seizures, heart attacks, and other conditions.
Successful Double-Blind Placebo-Controlled Study of Lithium for Acute Mania in Kids 7–17
Lithium is the treatment of choice for adults with bipolar disorder, but has rarely been studied in children or adolescents. One of the first double-blind placebo-controlled trials of lithium for the treatment of mania in children and teens aged 7–17 showed that the drug produced greater improvement in mania than did placebo. Side effects included blurred vision, abdominal pain, diarrhea, nausea, vomiting, fatigue, thirst, increased thyroid-stimulating hormone, decreased appetite, dizziness, sedation, tremor, increased urination, and rash.
In the study by researcher Adelaide S. Robb and colleagues, which was presented at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, doses began at 300mg twice a day, were based on each child’s weight, and were slowly increased.
At the same meeting, researcher Russell Scheffer presented data on 41 children who continued lithium treatment for 16 weeks with good results. The mean dose was 27.8 +/- 6.7 mg/kg per day.
Stem Cell Research May Help Explain Biochemistry of Bipolar Disorder
At the 2015 meeting of the International Society for Bipolar Disorders, researcher Martin McInnis described how stem cells can be used to identify biochemical abnormalities in patients with bipolar disorder. In this research, the stem cells, or IPSCs (for induced pluripotential stem cells), are created when cells from skin fibroblasts, which produce connective tissue, are treated with chemicals that cause them to de-differentiate back into stem cells.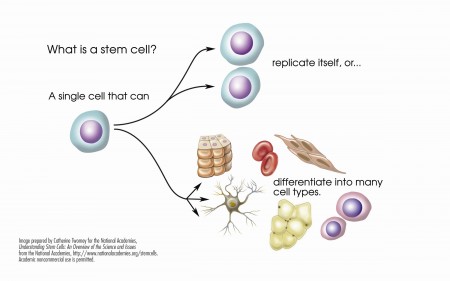
McInnis identified several abnormalities in the stem cells of patients with bipolar disorder. Stem cells with the gene CACNA1C, which is associated with vulnerability to bipolar disorder, fired more rapidly than non-CACNA1C stem cells. There were other abnormalities at the NMDA glutamate receptor and an imbalance of the neurotransmitter GABA in the cells. When the cells were treated with lithium, some of these abnormalities were reversed. In the cells with the CACNA1C gene, lithium normalized the firing rate. Lithium aslo re-balanced the distribution of GABA in the cells.
McInnis hopes that this stem cell research will shed light on the abnormalities associated with bipolar disorder, help explain how lithium corrects some of these, and lead to the development of new therapeutic approaches.
Lithium Safely Reduces Mania in Kids 7–17
The first large, randomized, double-blind study of lithium in children and teens has shown that as in adults, the drug can reduce mania with minimal side effects. The study by researcher Robert Findling was published in the journal Pediatrics in October. Lithium is the best available treatment for adults, but until now little research had been done on treatments for children and teens with bipolar disorder.
In the study, 81 participants between the ages of 7 and 17 with a diagnosis of bipolar I disorder and manic or mixed episodes were randomized to receive either lithium or placebo for a period of eight weeks. By the end of the study, those patients taking lithium showed greater reductions in manic symptoms than those taking placebo. Among those taking lithium, 47% scored “much improved” or “very much improved” on a scale of symptom severity, compared to 21% of those taking placebo.
Dosing began at 900mg/day for most participants. (Those weighing less than 65 lbs. were started at 600mg/day.) Dosing could be gradually increased. The mean dose for patients aged 7–11 was 1292mg/day, and for patients aged 12–17 it was 1716mg/day.
Side effects were minimal. There were no significant differences in weight gain between the two groups. Those taking lithium had significantly higher levels of thyrotropin, a peptide that regulates thyroid hormones, than those taking placebo. If thyroid function is affected in people taking lithium, the lithium dosage may be decreased, or patients may be prescribed thyroid hormone.