Alterations in Amino Acids in Blood That Affect Metabolism May Help Explain Chronic Fatigue
Chronic fatigue syndrome, more recently known as myalgic encephalopathy, is a debilitating and somewhat mysterious illness. However, a 2016 article in the Journal of Clinical Investigation Insight suggests that low blood levels of amino acids related to oxidative metabolism, the process by which oxygen is used to make energy from sugars, may play a role in the illness. High levels of amino acids related to the breakdown of proteins were also seen.
The study by Øystein Fluge and colleagues compared blood concentrations of 20 amino acids in 200 patients with chronic fatigue and 102 healthy participants. There were shortages in 6 amino acids that fuel oxidative metabolism in those with chronic fatigue, particularly women. Men with chronic fatigue had high levels of a different amino acid related to protein catabolism, the breaking down of complex molecules, a process that releases energy.
The differences between men and women with the illness might be because men use muscle tissue as a source for amino acids, while women, who have less muscle mass, use amino acids from blood as fuel.
The changes in both sexes suggest a functional impairment in pyruvate dehydrogenase (PDH), an enzyme that is important for the conversion of carbohydrates into energy. If PDH fails to work and cells turn elsewhere to create energy, muscles may suddenly weaken and lactate may build up, which patients experience as a burning in their muscles after the slightest exertion.
Fluge and colleagues are cancer researchers. They stumbled into chronic fatigue research when they noticed that people with chronic fatigue who were treated for cancer with the drug rituximab saw reductions in their fatigue. Rituximab, which is also used to treat some autoimmune diseases, is a monoclonal antibody directed at B cells. When it binds, it induces cell death. The researchers hope to clarify the link between the immune system and the problems with energy metabolism they have identified in people with chronic fatigue.
Measuring Inflammation in Neuropsychiatric Disorders May Shed Light on Treatment
Meta-analyses have found links between elevated levels of inflammatory markers and many neuropsychiatric disorders, including depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and traumatic brain injury. Multiple studies also show that those with elevated inflammatory markers such as interleukin-1, interleukin-6, tumor necrosis factor (TNF) alpha, and c-reactive protein (CRP) also respond less well to typical treatments than those with normal levels of these markers in the blood.
These links suggest that it could be useful to measure levels of these inflammatory markers in the blood of people who are responding poorly to medications. If one or more of these markers are elevated, it might be a sign that treatment with an anti-inflammatory agent could be helpful. Preliminary studies have shown that some neuropsychiatric disorders may improve after treatment with anti-inflammatory drugs such as aspirin, celecoxib (Celebrex), and the antibiotic minocycline, among others.
Blood and Now Brain Inflammation Linked to Depression
 There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
Common inflammatory markers that have been linked to depression include IL-6, TNF-alpha, and c-reactive protein. At the meeting, Meyer reviewed the findings on each of these. Twelve studies showed that IL-6 levels are elevated in the blood of patients with depression. Four studies had non-significant results of link between IL-6 and depression, and Meyer found no studies indicating that IL-6 levels were lower in those with depression. Similarly, for TNF-alpha, Meyer found 11 studies linking elevated TNF-alpha with depression, four with non-significant results, and none showing a negative relationship between TNF-alpha and depression. For c-reactive protein, six studies showed that c-reactive protein was elevated in people with depression, six had non-significant results, and none indicated that c-reactive protein was lower in depressed patients.
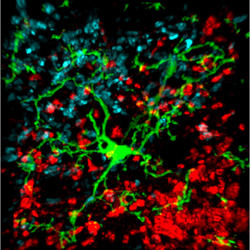
Most studies that have linked inflammation to depression have done so by measuring inflammatory markers in the blood. It is more difficult to measure inflammation in the brain of living people, but Meyer has taken advantage of new developments in positron emission tomography (PET) scans to measure translocator protein binding, which illustrates when microglia are activated. Microglial activation is a sign of inflammation. Translocator protein binding was elevated by about 30% in the prefrontal cortex, anterior cingulate cortex, and insula in study participants who showed symptoms of a major depressive episode compared to healthy control participants. The implication is that the depressed people with elevated translocator protein binding have more brain inflammation, probably via microglial activation.
The antibiotic minocycline reduces microglial activation. It would be interesting to see if minocycline might have antidepressant effects in people with depression symptoms and elevated translocator protein binding.
BDNF Is Decreased in Depression and Mania
Brain-derived neurotrophic factor (BDNF), which protects neurons and is necessary for long-term memory, can be measured in blood. In a symposium on bipolar disorder at the 2012 meeting of the Society of Biological Psychiatry, researcher Flavio Kapsczinski reviewed evidence from several meta-analyses showing that low levels of BDNF in the blood correlate with severity of an episode of depression or mania. In addition to the findings that BDNF levels are low during a mood episode, there are other reliable biomarkers of illness, including increases in intracellular calcium, increases in cortisol and failure to suppress cortisol by dexamethasone, and a variety of indices of inflammation and oxidative stress.
There are several common variants of the gene responsible for the production of BDNF, depending on which types of amino acids appear in its coding—valine or methionine. The Val66Val allele of proBDNF is the most frequently occurring in the population, and is the best-functioning variant. Those with a methionine substitution (Val66Met or Met66Met) have less efficient forms of BDNF. Researcher Jair Soares reported that the Met allele was associated with deficits in declarative memory in patients with bipolar disorder, and was also associated with smaller volume of the anterior cingulate gyrus.
Researcher Ghanshyam N. Pandey reported that patients with pediatric or adult bipolar disorder had decreased BDNF protein and mRNA levels in platelets and lymphocytes compared to controls. Treatment significantly increased these BDNF levels in the pediatric, but not in the adult bipolar subjects. These measurements in blood are consistent with findings that there are decreases in BDNF in the hippocampus and prefrontal cortex of patients who died while depressed or who committed suicide compared to controls.